The Short Term Effects Of Manual Handling Injuries

In our recent article, ‘The Devastating Effects Of Long-Term Manual Handling Injuries’ we discussed the long-term effects of manual handling injuries but what about the short term ones? What immediate effects will occur after suffering a manual handling injury?
To start off, the obvious thing to say is the pain, a lot of pain as you may know or even have experienced yourselves. Then depending on the injury, the emergency worker themselves may need to go to the hospital for emergency treatment which will cause distress, pain and time off work. This will affect not only their work colleagues but close friends and family too because they may no longer wish to socialise and do certain things whilst they’re recovering.
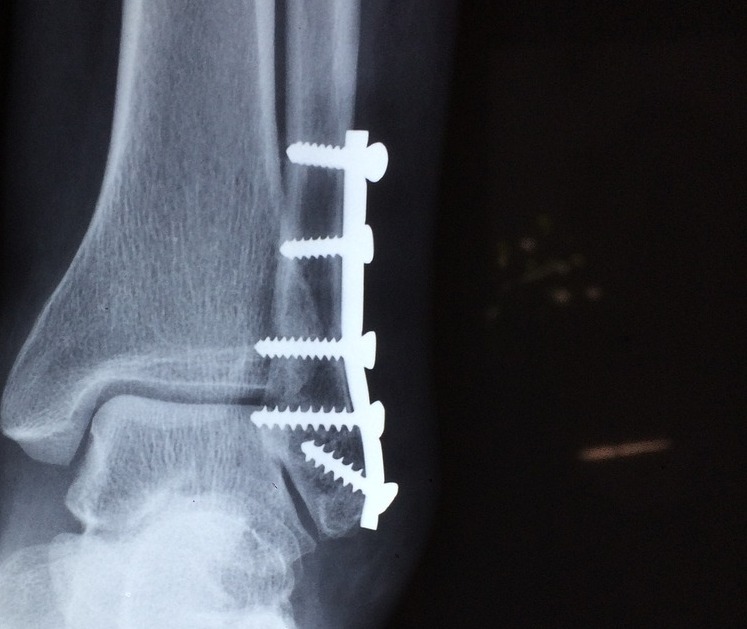
The type of injury could be anything from cuts, bruises, sprains, tears, small fractures to torn or strained muscles. A severe ankle sprain, for example, can take anywhere between twelve weeks to six months to recover from, especially with the chance of an operation and physiotherapy being needed. In fact, the Department of Labor found that out of a total of 14,470 manual handling injury cases reported 67% involved sprains or strains.
A major cut would need cleaning, a dressing and may need stitches and mean taking prescribed painkillers that could result in a short period of no longer being able to drive. A wound can also be at risk of infection and depending on where the injury is, there may be certain jobs that you can no longer do whilst you’re waiting for the cut to heal.

Another short-term effect that many of us who’ve experienced any sort of injury will know, is the lack of sleep and fatigue. When you’re in a lot of pain it can be difficult to sleep; the injury you have may force you to sleep in uncomfortable positions. This can lead to less concentration, headaches, dizziness and being in a bad mood or irritable. It can also lead to more serious injuries, for example, being tried whilst driving has been the cause of many car accidents.

One of the ways to stop certain manual handling injuries from occurring is with the correct emergency lifting devices. By having the appropriate equipment, it takes away the need for the emergency worker to manually lift a fallen patient up.
We can help prevent some of the manual handling injuries that are frequent amongst emergency service workers with our emergency lifting cushions, such as, the Mangar ELK or Mangar Camel. Chris Lokits, a quality assurance officer at the Louisville Metro EMS explained how our lifting cushions have been “a blessing.”
“When doing a lift assist by myself I am confident that I can successfully get the patient up without hurting them or myself. With a decrease in IODs and workman’s compensation claims, I believe this device will soon pay for itself. It’s invaluable. “ he explained.
If you’re interested in finding out further information regarding the Mangar Camel or ELK or would like to request a free product please click here.
7 Red Flags Of Early Onset Dementia

Have you been noticing differences in yourself or someone close to you? Have you noticed subtle changes in memory, mood swings or maybe finding it harder to find the right words? We understand that contemplating the fact you or a loved one could have early-onset dementia is a scary thought and because of that, you may subconsciously try to dismiss and deny the early signs as something else entirely.
Identifying the early stages of dementia can help slow down the progression and that’s why if you notice any of the following seven symptoms we would urge you to go and speak to your GP and get some medical advice immediately.

7 Early Symptoms
-
Lapses in Memory
The first changes you may have noticed are lapses in short-term memory. We all know that everyone has the occasional moments where they might’ve forgotten something however it isn’t the same if it’s happening frequently. People with early onset dementia may forget what they had for their lunch but can still remember memories from their childhood. It may be that you have forgotten where you left something, forgotten important dates or events, forgotten how to make something you usually know how to do or retell a story which you’d only just finished moments ago.
-
Confusion
Whilst in conversation you/they may find it difficult to find the right words and it might always be on the ‘tip of the tongue’. This can cause frustration and you may swap the word for something like ‘thingamajig’. Again, these things may sound like something that we all have done but if it’s a frequent occurrence and you’ve consciously noticed it then there could be a problem developing.
-
Mood Swings
Unfortunately, as dementia develops you may find that you/they suffer from severe mood swings. A conversation or situation can rapidly make a person change from being happy to angry in a matter of seconds and for no obvious reason and they may become more argumentative. Alternatively, they may show less emotion or if they’re usually shy it’s not uncommon that they will become more outgoing.
-
Loss Of Interest
You may have found that you’ve lost interest in things you were usually passionate about, whether that was a hobby or spending time with friends or family etc. It may seem like they don’t want to do anything anymore and sleep more than usual.
-
Lacking Sense Of Direction
In the early stages, it’s common that sense of direction will begin to deteriorate, meaning that you may be finding it hard to remember familiar landmarks and forget your way to and around certain places that you’ve regularly gone to before. It’s also harder for them to follow step-by-step instructions and directions.
-
Repetition
It’s common due to the memory loss associated with dementia that you may have noticed your loved one beginning to repeat themselves in conversation, like asking the same question even when it had previously been answered. They may also start to repeat daily tasks such as shaving or washing their face etc.
-
Struggle to complete normal tasks
You could’ve noticed that your ability to perform everyday tasks may have become more difficult, like following a recipe or you may find that find particular games you used to enjoy hard to follow, especially if there are a lot of rules. You may find that it’s also harder to learn how to do new things and follow different routines.
Another common thing associated with dementia is the propensity to fall frequently.
The Mangar Camel Lifting Cushion allows a fallen person to be lifted safely and quickly off the fall and keep stress to a minimum. If you’d like more information regarding the Camel please click here.
If you’re unsure and worried about what to do then please read our ‘Where To Get Help If You Think You Or Someone Is Living With Dementia’ article here.
Where To Get Help If You Think You Or A Loved One Is Living With Dementia

If you’ve noticed that either you or someone close has been showing the early symptoms of dementia you should encourage them to go and speak to their GP and talk about the possibility that you or they could be developing dementia.

If you’re unsure of the symptoms you can find them in our ‘7 Red Flags Of Early Onset Dementia’ here.
What is Dementia?
You might be thinking ‘but what is dementia?’ Dementia occurs when nerve cells in the brain begin to die. As more and more cells disappear the brain begins to shrink, causing the symptoms of dementia, which disrupts your memory, thinking, problem-solving and changes in your overall mood.
How to tell someone you think they’re showing signs of dementia
You may not want to hurt your loved one’s feelings or are worried that if you mention your concerns they’ll be offended or angry. It’s important to know, however, that even though there’s no known cure for dementia if it’s detected early, then in some cases its progression can be slowed down through certain treatments.
The Alzheimer’s Society suggests that you do the following when approaching someone with your concerns:
- Choose to have the conversation in a place that’s in a familiar environment.
- Explain that you’re bringing up your concerns because you care and that it was important for you do so because communicating is important.
- Use examples to make things clearer: it’s important not to create a sense of “blame”, for example, instead of telling someone they couldn’t make a cup of tea, you could suggest that they seem to find it difficult to make a cup of tea.
- Have an open conversation and be honest and direct – for example, ask how they’re feeling about their memory.
- Make a positive plan of action together.
What to expect when speaking to your GP about early onset dementia?
A dementia diagnosis is usually given after a GP has ruled out all other possible conditions. The GP will examine you or your loved one and will run a series of assessments and tests to see whether there are any other reasons as to why the symptoms might be occurring.
It’s possible that the symptoms could be related to the current medication being taken, deficiencies in vitamins and minerals or a urinary infection.
After ruling at all other avenues and seeing a slow progression of symptoms that get worse over time than a diagnosis of early onset dementia may be made. If so a referral may be made to a Memory Service who will provide an assessment, diagnosis and ongoing support and information for you and your carers. (please bear in mind this will be different to the area you live in).
Will everything be ok?
In upsetting circumstances such as these, the best thing to do is keep an open flow of communication with your family, friends, and GP. Your GP will give the best advice on available treatments and methods to help slow the onset of dementia and your friends and family will give you the emotional support you need.
You may find our article, ‘5 Simple Tricks To Stop The Onset Of Dementia’ of importance so please click to find out more here.
Unfortunately, people with dementia have a greater propensity to fall over frequently. Our Camel Lifting Cushion allows the person who has fallen to be lifted safely, quickly and keeps the associated stress to a minimum. The cushion is designed to allow the person living with dementia to be able to stay at home by giving their caregivers the aids they need to keep them safe.
If you’re interested in finding out further information regarding the Camel please click here.
Tips On Visiting A Loved One Living With Dementia


A recent survey carried out by the Alzheimer’s Society showed that 42 per cent of the public thought that maintaining contact with someone living with dementia, who could no longer remember them, was pointless.
Have you struggled with the thought of visiting a loved one living with Dementia and been unsure whether to do so or not? Have you ever sat at your laptop and googled, ‘How to visit someone with dementia’ or ‘how often should you visit someone with dementia’, maybe you’ve even googled ‘Should I visit someone with dementia if they don’t know who I am’.
When you’ve got a loved one living with dementia, it can sometimes be hard to come to terms with it and the idea of a visit may be a daunting.
The Alzheimer’s Society carried out a survey on 300 people living with dementia and found that 64 per cent felt lonely and isolated from their friends and family. This can lead to feelings of isolation and cause patients to withdraw from society. The survey found 54 per cent no longer socialise or participate in activities.
The Alzheimer’s Society urge people to maintain contact with loved ones living with dementia and remember that even if they can’t remember your visit, it will still reduce feelings of loneliness and bring them happiness.
To help you next time you visit your loved one, we’ve put together some tips and advice.
Tips to help when visiting a loved one with Dementia:
- Approach from the front and not from behind.
- Introduce yourself when you first greet them, ‘Hi Nan, I’m Liz your granddaughter.’
- Maintain eye contact.
- If you’re not recognised, as upsetting as that can be, try to stay smiling as it will reassure the person you’re visiting.
- Be patient and listen.
- Limit visitors to 1 – 2 people at a time, as you don’t want them to feel overwhelmed.
- Visit at a time of day you know they are usually at their best and not tired.
- Try to be positive and reassuring.
- Be prepared for them to make incorrect statements or to say something that’s unpleasant to hear. Never take it personally.
- It’s both normal and perfectly OK to feel a wide range of feelings during your visit.
Be aware you may hear some upsetting things from your loved one like, ‘I want to go home’ or ‘please take me with you’. The best way to react is to reassure them, be patient with them, and confirm their value as a person and as a member of your family or friend.
Whilst visiting we suggest you take things which may be familiar to them, like their favourite chocolate, play a card game, listen to familiar music or read them a book aloud.
If you know someone who is living with dementia, or you are living with the condition yourself please feel free to leave us your thoughts and comments below.
People with dementia have a greater propensity to fall over. The Camel Lifting Cushion allows a fallen person to be lifted safely, quickly and keeps associated stress to a minimum. This is because the user can keep their feet on the ground and they feel more secure.
If you’re interested in finding out further information regarding the Camel please click here.
5 Simple Tricks To Stop The Onset Of Dementia


Unfortunately, we may not be at the stage where we have a cure for Dementia, but that doesn’t mean we should lose hope. We should continue to fight it and try to slow down the onset.
There are an estimated 50 million people living with Dementia worldwide, the number is estimated to double every 20 years.
What is dementia?
Dementia occurs when there is a loss of nerve cells in the brain and when a nerve cell dies, it cannot be replaced. As more and more cells begin to die the brain starts to shrink causing symptoms which include problems with memory, thinking, problem-solving, language, visual perception and changes in mood.
Dementia is brought on by previous infections which affect the brain, like strokes and Alzheimer’s disease. It is not a natural part of ageing and will progressively become worse.
Recent research shows…
- Earlier this year, U.S. researchers warned that dementia rates will triple by 2050 if we continue to live unhealthy lifestyles.
- Boston researchers found that a fast-paced walk could hold the key to slowing the onset of Alzheimer’s and Parkinson’s in later life.
- Professor June Andrews has found that certain vitamins, such as B6 and E, have been shown to cut the risk of Alzheimer’s.
5 Simple Tricks To Fight It
Keep physically active
It’s important to be physically active for at least 30 minutes a day, five times a week. Regular physical exercise in middle-aged or elderly people reduces the risk of developing dementia because it makes your heart and blood circulatory system more efficient.
Exercise will lower your cholesterol and keep your blood pressure at a healthy level which in turn decreases your risk of developing dementia.
Why not take up swimming, yoga, walking, cycling, join an exercise or a dance group today?
Eat a healthy balanced diet and don’t smoke!
A healthy and balanced diet includes all the main food groups but in certain moderations. Try to eat high proportions of oily fish, make sure you’re having your 5-a-day of fruit and vegetables, cook with olive oil and eat low amounts of red meat and sugary treats.
It’s also important to cut down on saturated fats, such as cakes, biscuits and cheese and keep an eye on your salt intake.
Your choice of food is so important to ensure you’re healthy! What you decide to eat helps to determine whether you have low cholesterol and low blood pressure and therefore reducing your risk of dementia, a stroke or diabetes.
Don’t smoke! Smoking harms your lungs, heart and blood circulation which results in a greater risk of developing dementia. It can also cause your arteries to narrow which leads to a rise in your blood pressure.
If you currently smoke and would like to quit, please speak to your GP who can provide help and advice about quitting.
Exercise Your Mind
Keeping your mind active will likely reduce your risk of dementia. Research has found that keeping your brain active will help to build its reserves of brain cells and make connections stronger.
Try reading, learning something new like a different language, doing puzzles like word searches or crosswords, playing cards games with friends, or begin a new hobby.
All of the above makes your brain need to restructure and rewire itself to help keep up with the new demands placed on it. Therefore constantly being tested and needing to adapt making it healthier and not becoming idle.
Have a snooze in the sun (remember your sunscreen!)
Sleep is so important to help maintain our bodies are healthy and happy. It can impact your mood for the day, your memory, your thinking capability and is vital for your mind’s health.
On the other hand, a researcher has linked vitamin D to help minimize the risk of Alzheimer’s and therefore Dementia. We get most of our Vitamin D from the Sun. Scientists at the University of Southern California, Los Angeles found that Vitamin D may be responsible for activating cellular signalling that clears the brain of plaque build-up and low vitamin D levels are linked to poor brain power.
Life’s too short to stress
Stress can have a huge negative impact on our body and affects the immune system which is known to play an important role in the development of dementia. The hormone cortisol is released when severely stressed and this has been linked to problems with memory.
It’s important to surround yourself with people and things you love and enjoy! Staying social keeps your mind active and stimulated but also helps when suffering from stress.
Try meditation, deep breathing, socialising with friends, exercising and relaxation techniques to reduce your level of stress.
Sadly, people with dementia have a greater propensity to fall over. The Camel Lifting Cushion allows a fallen person to be lifted safely, quickly and keeps associated stress to a minimum. This is because the user can keep their feet on the ground and they feel more secure.
If you’re interested in finding out further information regarding the Camel please click here.
If you know someone who is living with dementia, or you are living with the condition yourself please feel free to leave us your thoughts and comments below.
Dementia Symptoms Subside When Maternal Instincts Take Over


Morleen Templeman is 83 years old and living with dementia. As part of her dementia, Morleen finds it difficult to clearly communicate with her carers at the Faiross Village in the northern New South Wales town of Bangalow in Australia.
Manager Jo Dwyer explains, “One of the biggest ways Morleen has been affected is her speech. She’ll be muttering and unable to say anything clearly, but very occasionally she might say ‘thank you’ or ‘pretty flower’.
So what is dementia? Dementia is caused by the loss of nerve cells in the brain and unfortunately, when a nerve cell dies, it cannot be replaced. As more cells begin to die the brain starts to shrink causing symptoms which include problems with memory, thinking, problem-solving, language, visual perception and changes in mood.
Dementia isn’t a disease in its own right and is brought on by previous infections which have affected the brain, such as strokes and Alzheimer’s disease. It’s not a natural part of ageing but is a progressive condition so it will get worse.
However, Morleen’s condition changes when a special visitor arrives at the Faiross Village in the shape of carer Shelly Fletcher’s six month-year-old daughter, Lola.
Shelly Fletcher explains, ‘Since we welcomed Morleen into the village her journey has been quite difficult. It is incredible to see the transformation in Morleen when Lola is around. ‘
Manager Jo Dwyer says, ‘ Memories can be triggered in a variety of ways but for many women who have been mothers themselves, nothing beats a cuddle with a baby. I think it’s that long term memory recognizing the maternal love that she will have had her own children and grandchildren ’
Researchers have been trialling and looking into Doll Therapy (DT) since the first study by Milton and MacPhail in 1985 as an effective method of intervening the symptoms of dementia.
A key researcher describes Doll Therapy as a “wise and mindful use of dolls for their symbolic significance to help improve the well-being of people with dementia” (Verity 2006 p.27).
On a global scale, DT research has been expanding and in a positive direction which has identified four main outcomes; it helps elderly people with dementia to do the following:
- Initiate and encourage interaction and communication
- Fulfills attachment and nurturing needs
- Acts as a transitional object
- Provides sensory stimulation through activity
(Mackenzie, Wood-Mitchell and James 2007).
Alander, Prescott and James (2013) witnessed participants carry, feed and dress the dolls which showed their maternal and paternal instincts and nurturing tendencies had not been affected by the effects of living with dementia.
Faiross carer, Shelley Fletcher continued,’When Morleen sees Lola her whole body changes and she puts her hands out like she wants to hold Lola. Her speech improves and she starts to talk in sentences. We naturally both start caring for Lola and she’ll start changing her nappy and things like that.’
It’s not just the residents who benefit from Shelley Fletcher bringing her baby to Faiross Village, as a helping hand is always welcome.
Carers are urging fellow mums to also to bring their children to visit the elderly as it’s a joy for all involved, and especially for those living with dementia.
Sadly, people with dementia have a greater propensity to fall over. The Camel Lifting Cushion allows a fallen person to be lifted safely, quickly and keeps associated stress to a minimum. This is because the user can keep their feet on the ground and they feel more secure.
If you’re interested in finding out further information regarding the Camel please click here.
If you know someone who is living with dementia, or you are living with the condition yourself please feel free to leave us your thoughts and comments below.
Outdated Manual Handling Practices Causes Rise In Injuries To Paramedics


Emergency care has been recognised for many years as exposing ambulance workers to high risks of musculoskeletal injuries. Paramedics are especially known to report a high level of musculoskeletal injuries, particularly from patient moving and handling.
“MSK most common occupational disease in Europe”
(European Agency for Safety and Health At Work)
Across Europe, the job role of an ambulance worker may differ, however, the evidence is compelling that all ambulance workers are at a high risk of an early retirement due to health problems such as musculoskeletal disorders.
Manual handling injuries cover a broad category of work related injuries but can include injuries due to lifting, trapped fingers, cuts from sharp objects and pushing and pulling etc. The most common manual handling injuries are MSDs or musculoskeletal disorders, which are injuries and disorders that affect the human body’s movement or musculoskeletal system.
Many ambulance workers are still performing outdated manual handling manoeuvres instead of using modern lifting devices, such as the Mangar Camel and Mangar ELK leaving them exposed to musculoskeletal risks, for example when trying to lift a patient from the floor or when moving them from a stretcher to a bed.
“Every year millions of European workers are affected by MSDs through their work”
(European Agency for Safety and Health At Work)
Work-related lower back pain is the most common musculoskeletal disorder caused by manual handling and a quarter of workers across Europe have reported suffering from back pain due to their work. The European Agency for Safety and Health regard back pain as one of the top work-related disorders. Data taken in a European survey on working conditions found that 30% of European workers suffer from back pain, which tops the list of all reported work related disorders.
The recent figures from the European Survey on working conditions (ESWC) showed that 24.7% of European workers complain of a backache, 22.8% of muscular pains, 45.5% report working in painful or tiring positions while 35% are required to handle heavy loads in their work.
In 2013, a paramedic in England was awarded compensation because his back and shoulder were left with permanent damage after trying to manoeuvre a patient into the back of an ambulance in a carry chair with no fitted tail lift.
The 53-year-old sustained injuries that meant he was off work for four and a half months after carrying out the awkward manoeuvre which exacerbated an existing back injury.
“As paramedics, we do get back and shoulder injuries fairly frequently due to the nature of the job but the risks of them and their severity can be minimised by management giving us the correct tools to do the job safely,” said the paramedic.
Musculoskeletal disorders are preventable with the correct training and equipment and so are the economic and human costs of MSDs.
In the UK, ambulance services now carry a Mangar ELK or a Mangar Camel. They are both emergency lifting inflatable cushions designed to provide a safe and dignified for the patient and also to protect the ambulance worker from having to manually lift the patient.
“Our team use a Mangar Lifting Cushion to raise the fallen person from the floor. The cushions provide a safe lift for the resident but also help prevent musculoskeletal injury to our staff. Because of a number of falls we attend, the lifting cushions are used every day and have been for nearly 10 years. They are a reliable piece of equipment that we wouldn’t be without.”
Heather Rimmer, Norfolk Swift Response
If you would like any further information regarding the Mangar Elk or the Mangar Camel, please click here.
New Mangar Distributor Lifted By Heart-Warming Moment


When your job is to promote life-changing products like those designed and manufactured by Mangar Health, there can be emotional moments helping people with limited mobility retain their independence.
Nils-Christian Fjaebu, our new distributor in Norway was excited to begin selling Mangar products but was taken by surprise when he experienced a heart-warming moment with a client so soon after being appointed.
Nils-Christian had been asked to demonstrate a Mangar ELK to a young lady who was paralysed from the waist down. She had been living independently but was finding transferring from the floor into her wheelchair or to a seated position, more and more difficult.
Nils-Christian explained, ‘When I arrived to meet the young lady involved I knew the Mangar ELK lifting cushion would be of benefit to her but I didn’t realise just how much.’
He continued, ‘I am a strong advocate of the ELK after seeing with my own eyes the difference it can make to someone’s life.’
The Mangar ELK is an inflatable emergency lifting cushion is designed to deliver a dignified and safe lift. It can easily be used in confined spaces and is regularly prescribed in home environments across the UK.
Nils-Christian said, ‘After demonstrating the Mangar ELK it wasn’t long until the patient was having a go herself and quickly took to the product. She was using it independently to help her get up and off the floor and into her wheelchair. It was a delight to see.’
The patient had also explained how she had never been able to enjoy the simple pleasure of sitting on the grass and enjoying a picnic during the summer with her friends. Even with friends or family to help her up she still had difficulties.
Nils-Christian concluded. ‘It was so emotional to see how the Mangar ELK would change her life and witness how happy she was to find a piece of equipment that was so easy to use.
‘I’m looking forward to working with Mangar in the future and promoting products that I am confident will change many lives for the better.’
If you would like to see more information regarding the Mangar ELK or are interested in becoming a distributor, please click here.
The Perfect Diet For People Living With Arthritis

At Mangar Health, we have seen many of our customers’ living with the effects of arthritis and it got us thinking into whether there was an ‘ideal’ diet for people living with the condition.
Keeping an eye on your diet is so important when you suffer from arthritis. It is important that you are getting the correct vitamins and minerals you need, whilst steering clear from certain foods which are known to increase pain and discomfort.
A diet which is low in processed food (high in omega 6) and rich in fruit, vegetables, fish (high in omega 3) and whole grains has been shown to help fight inflammation and boost your immune system, which is a perfect combination for people living with arthritis.
A diet that is similar to the Mediterranean diet which is renowned for having disease fighting properties is beneficial for those with arthritis.

We have put together some meal ideas, which you could be eating for breakfast, lunch and dinner which includes important ingredients to help with arthritis.
Breakfast
- Smoked mackerel on whole grain toast.
Experts recommend at least two portions of fish twice a week. So having mackerel for breakfast is a great way to make sure you start the day off right with a dish full of those important anti-inflammatory omega 3’s.
- Scrambled eggs, avocado and smoked salmon on whole grain toast.
Eggs are packed with protein and vitamin B’s so they’re another great way to start the day! Combine them with avocado which is absolutely bursting with vitamins and minerals (20 to be exact) and finish with a bit of smoked salmon on top … yum!
Lunch
- Broccoli and Spinach Soup
Research has shown that vegetables which are rich in vitamin K reduce inflammatory markers in the blood dramatically. Therefore a soup which contains vegetables such as broccoli, kale, spinach and Brussel sprouts are a must!
- Roasted red pepper and chicken wrap
Vegetables and fruits that have a darker or more vibrant colour are known to have more antioxidants. Peppers are high in Vitamin C, antioxidants and have anti-inflammatory properties. Add a bit of grilled chicken for protein and some lettuce for your vitamin K and you have a delicious lunch.
Dinner
- Chicken Tikka Masala
Indian dishes are full of delicious flavour and packed with spices and ingredients which not only taste good but are good for your body. Spices such as turmeric, ginger and garlic which are used frequently in a majority of Indian cuisine are packed with anti-inflammatory properties and are a good choice for those living with the condition arthritis.
- Chilli Con Carne
Enjoy a delicious chilli con carne packed with red kidney beans. Red kidney beans were ranked in the U.S. Department of Agriculture’s top four antioxidant-containing foods. Beans are an excellent source of protein and are loaded with fibre. Combine with whole grain rice and you’ve got another yummy meal to tuck into.
There are loads of recipes out there waiting to be tried, just remember to keep a balanced diet and ensure you are including fish, nuts & seeds, fruit & vegetables, olive oil, beans and whole grains.
If you’re living with the condition of arthritis and looking for further ways to help cope with your condition then you may find the Manager Bathing Cushion useful and helpful. If you would like further information then please click here.
Six Top Tips On How To Reduce Arthritis Pain

There are around 350 million people who suffer from arthritis worldwide. Arthritis causes painful inflammation of the joints and unfortunately, there is currently no known cure for the disease. However, here at Mangar Health, we have put together some tips to help reduce the pain and make living with arthritis bearable.
Mediterranean Diet
There are so many delicious foods out there that can help fight pain and inflammation which so many arthritis sufferers endure. The Arthritis Foundation recommends a Mediterranean diet or appropriately renamed ‘The Ultimate Arthritis Diet’ which contains all sorts of foods from fish, nuts & seeds, fruits & vegetables, olive oil, whole grains and beans. The diet emphasises foods that are rich in omega fatty acids.
Omega-3 fatty acids which are in fish and olive oil among other things are known to help reduce pain in arthritis. The University of Maryland Medical Centre found ‘that omega-3 fatty acids reduce inflammation and may help lower risk of chronic diseases such as heart disease, cancer, and arthritis.’
It is also important to know the difference between omega-3 and omega-6 as omega-3 fatty acids are known to reduce inflammation, whilst on the other hand omega-6, fatty acids tend it promotes inflammation instead. High levels of omega-6 tend to be found in food such as vegetable oils, fast foods, dairy and eggs etc.
To see a list of foods that contain high levels of omega-6 fatty acids click here.
To see a list of food which contain high levels of omega-3 fatty acids click here.

Exercise, Exercise, Exercise
Exercising is so important for people living with arthritis because it helps build strength, increase flexibility, fights fatigue and reduces pain. Whilst, we don’t recommend going for long runs or lifting weights as this will cause more damage than good, the idea of exercising while already in pain isn’t the most pleasant idea. We do recommend, however, that you do low to moderate exercise as this can make such a difference in your overall wellbeing and reduce pain and symptoms of arthritis.
Even though you might think that exercise will irritate your joints and cause further pain and stiffness this isn’t the case at all! In fact, a lack of exercise can make your joints and pain even worse. This is because without exercise your muscles and surrounding tissue will become weaker and no longer be able to continue supporting your bones and therefore will increase stress on your joints.
Please remember to always double check with your doctor before starting any new form of exercise.
Use Hot and Cold Therapy
Hot therapy is a good way to reduce arthritis pain because heat enhances circulation and helps nutrients to be delivered to your joints and muscles quicker.
A long hot bath is an effective way to help ease stiffness in your joints especially in the morning when you’re more likely to be stiff. It is also a good idea to have a warm bath before you go to sleep, it will help reduce pain and therefore help you get a better night’s sleep.
On the other hand, getting in and out of the bath whilst in pain and stiff can be rather daunting and you may feel that it is rather uncomfortable. If this is something you struggle with then the Mangar Bathing Cushion may be able to help you with this.
“They say Miracles seldom happen but for me, the Mangar Bathing Cushion is one. Increasingly crippled by Arthritis I found it agony to climb into my ancient narrow bathtub but now I can sit comfortably back and be lifted into the bath and when I am ready lifted out again. It does all the work for me in blissful comfort.” – Mrs Jackson
You can continue the hot therapy with an electric blanket in your bed or by placing a heating pad in the more painful areas at night to continue to keep your joints loose.
Cold therapy is usually used to help reduce acute arthritis pain because it slows circulation and reduces swelling. A cold compress such as an ice pack or a bag of frozen vegetables can be used to numb nerve endings and help to dull the pain for a quick relief.

Massage Therapy
In a recent study, the Arthritis Foundation found that having a massage on a regular basis, especially targeting the arthritic joints, can help to reduce pain and stiffness and increase flexibility. Research has shown that a massage lowers the body’s production of a stress hormone called cortisol and increases the production of serotonin which is known to reduce depression, heal wounds and maintain bone health and therefore increases your mood. As a massage also helps to reduce pain this will improve your sleep as a result.
If you’re worried about the cost of frequent visits to a massage therapist you can work with a physical therapist to learn how to self-massage which is just as effective.
Weight loss
Weight is an important factor regarding an increased amount of pain from arthritis, as excess weight results in an increased pressure on your joints and therefore results in heightened pain and inflammation.
Rich F. Loeser Jr MD, a rheumatologist at the Thurston Arthritis Research Centre explains how weight gain is a key factor affecting arthritis pain – “even more importantly, the number of inflammatory mediators produced in fat affects joint tissues and plays a role in pain”.
Weight gain can be linked to an increase in arthritis pain, weight loss, therefore, may help to improve arthritis symptoms as there will naturally be less pressure and excess weight on your joints resulting in less wear and tear.
Herbal Medicine
Herbal medicines are also another great treatment to help reduce pain as certain herbal remedies contain anti-inflammatory and painkilling properties. They are also known to help improve energy and help sleep. A few popular herbal medicines that have proven to be effective in reducing pain in arthritis is devil’s claw, Boswellia and rosehip amongst others.
Please remember to speak to your doctor first before taking any medicine that hasn’t been prescribed.
If you suffer from arthritis and know of any other techniques that have helped you to cope and reduce the pain then let us know or if you’re interested in finding out more information regarding the Mangar Bathing Cushion then please feel free to contact us here.
8 Top Tips For Travelling With A Disability

Here at Mangar Health, we’re passionate about ensuring everyone gets to live a full and exciting life. With that in mind, we’ve been speaking to Rob from The Bimblers about his top tips for travelling with a chronic illness or disability…
If you are anything like us, you already know how hard life can be when you’re living with a chronic illness or disability. It never leaves you, it’s the architect of everything you do and it zaps your enthusiasm for an active life but it doesn’t need to be that way.
We all know, we’re unlikely to become pain-free or shake off the chains of our chronic illnesses and disabilities. So we adapt, we learn to live with it and figure out another way to thrive, to enjoy our lives despite our illnesses and that’s what I want to share with you in this post.
Our escape from chronic illness is travel. Both Bridget and I have illnesses that limit our ability to travel but instead of using them as an excuse, we treat them as a challenge.
For us, travel makes us happy, it’s where we are our old selves and where we can momentarily forget about our daily challenges.
We know it’s hard travelling with a chronic illness or disability, we know there will be times when travel is impossible and we also know it’s often easier to do nothing. We get it, but here’s the thing, on the flipside, travel can be liberating, exciting and an opportunity to escape, even for a short time.
Travel can often seem like a challenge too far. With that in mind, let us share our top tips for travelling with a chronic illness or disability. These tips won’t remove all of your barriers, but what they will do, is give you the chance to stack the deck in your favour.
Travelling with Chronic Illnesses and Disabilities
Start with the Right Attitude
Attitude is often overlooked when we talk about travelling. What we mean by attitude is how you view travel, is it a chore, scary, too difficult or is it something to look forward to, exciting and a welcome relief from the norm?
If you start with the attitude “Where There’s a Will There’s a Way” then despite your reservations, travel can become one of the most rewarding activities for both your physical and mental health.
Another aspect of having the right attitude is what you actually view as travel. For some, travel means going abroad, laying on a beach or cruising the seas in a luxury cabin. For others, travel means going for a walk in a local park, visiting a neighbouring town, taking a staycation and everything in between.
The point is, travel can mean whatever you want it to mean. If travelling abroad sounds scary, start with a day out in your own backyard. We love a walk along the promenade or through a local country park.
One you have one or two successful days out under your belt you’ll be surprised how your attitude to travel changes. Once you’ve proven to yourself that you can do it, you can then move onto an overnight stay in an accessible hotel or a weekend away in an accessible cottage.
Plan Then Plan Some More
As a person living with a disability or chronic illness, you’ll already be used to planning. It seems our whole lives revolve around planning and never more so when it comes to travelling.
Most tourism destinations, holiday companies and accommodation providers have access information on their website. Then there is first-hand information from travellers such as ourselves on The Bimblers, the national accessible tourism charity Tourism for All and sites like Euan’s Guide.
When we plan a trip, we start with the official tourism department website then use Euan’s Guide and Facebook groups to look for people who’ve actually visited. This way, we are able to fill in the gaps of information not available on the official site.
These days, there is so much information available online but only you know the specific details you need to make an informed decision about whether your chosen destination or activity is right for you?
Another thing about planning is to expect the unexpected. The truth is, things go wrong, they always do whether you’re disabled or not.
It’s impossible to plan for every eventuality, which takes us back to attitude. When you travel, it’s not what goes wrong, it’s how you deal with it and that leads us nicely onto our practical tips for travelling with a chronic illness and disability.
Practical Tips
Prepare
Make sure you have enough medication to last your whole trip. Ideally, have some kind of documentation detailing your conditions and proof of needing to carry medication.
Whether you’re travelling in the UK or abroad, make sure you know where the nearest Doctor or Hospital are located. If you are travelling abroad, make sure you know where there’s an English speaking Doctor.
Very important, make sure you have adequate travel insurance and contact numbers should you need to use it.
If you use equipment such as a wheelchair, where can you get spare parts or repairs if it breaks? Can you hire aids or equipment locally?
Accommodation
Depending on your condition, is your holiday accommodation suitable? Don’t wait to get there to find out and despite what we said earlier, don’t believe everything you read on the internet.
Contact the accommodation directly, ask specific questions about access, ask about facilities both in your room and in the rest of the hotel.
If you need to know how wide the door is, how high the bed is or what evacuation procedures are in place, don’t be afraid to ask.
If you need to take your own mobility aids or hire them in, check in advance that your accommodation provider allows them. Check to see what equipment they already have in place and if there are any additional charges to use them.
Transport
If you’re using public transport, is it accessible?
If you’re flying, what policies do the airline have in place for passengers carrying medication or mobility equipment? What assistance is available to help navigate the airport, help you board the plane and disembark?
Can you use the toilet on the plane, can you get up and move around if you get too stiff? What are your rights if something goes wrong, you’d be surprised how many airlines lose bags or damage wheelchairs.
Excursions
If you like exploring, check in advance that the places you want to visit are accessible. If you’re driving, what’s parking like for disabled drivers, are there any concessions for blue badge holders?
If you’re going on a guided tour, make sure the tour will move at your pace. If you’re accompanied by a carer, are there any discounts available for carers? Many tourist attractions offer discounts or free entrance for carers.
Rest
Build downtime into your travels. When you’re on holiday it’s tempting to rush around and try to cram everything in – don’t! Take time to relax, listen to your body because it’s the best measure of how much or how little you should be doing.
If you need to take a day off when you’re travelling don’t feel guilty just rest up and look forward to the next day.
Travel Should Be Fun
Whenever we read tips about travelling with a chronic illness or a disability, they generally talk about the practical side of travelling, much like we did above. But, they inevitably forget to mention the most important travel tip – have fun.
Travel should be a pleasurable experience, there is little point in worrying about things that haven’t happened yet because it takes the fun out of it.
Once you’ve done your planning, made your arrangements and prepared yourself to have a good time, let yourself do exactly that – allow yourself to have fun.
If you would like to find out about how Mangar Health can assist you when travelling if you’re living with a disability, please get in touch with our sales team who will be more than happy to help.
About The Bimblers
Rob and Bridget are the bloggers behind the successful travel blog TheBimblers.com. They share personal stories of travelling in a wheelchair, overcoming the barriers of travelling with Rheumatoid Arthritis and Fibromyalgia and they actively promote good disabled access in the tourism industry.
Twitter – @TheBimblers
Facebook – The Bimblers Blog
The Beginner’s Guide To Working In A Care Home

We’ve been talking a lot recently about what it’s like to work in a care home.
As part of that we had spoken to our followers on Facebook, Twitter and LinkedIn who were working in the industry to find out what they thought were the best and worst parts of their jobs were.
Looking back though, it occurred to us that we may not have given a fully reflective view on what is a truly rewarding profession to work in. With that in mind we went back over all the responses we’d had in and combined them into the below; listing the seven top reasons working in a care home will be one of the most meaningful jobs you’ll ever do…
It’s A Privilege To Make A Difference
Without sounding too gushy (as we do appreciate how hard a job it is), a career working in a care home will be one of the most rewarding things you’ll ever do. There aren’t many jobs in which you can say you make a daily difference to someone’s life, taking care of the residents and giving their families the peace of mind knowing their loved ones are looked after.
You Can Be Flexible
On a slightly more practical level, care home workers are needed at all times of the day and night which means this is the ideal industry for someone looking for a bit of flexibility in their shifts. Whether you’re a student, trying to balance a work life around the kids, just returning to work or even semi-retired, a care home will no doubt be able to accommodate the shift patterns you need.
You’re Part Of A Team
Working in a care home you’ll be part of an interdisciplinary team providing physical therapy, case management and much, much more. Between you and your colleagues you’ll need to work out and implement care plans for the residents.
This reliance on team work will give even the most junior members of staff exposure to a wide range of skill sets with the comfort of a highly qualified team backing them up.
Providing Companionship To Those Who Most Need It
Numerous studies over the years have repeatedly shown that socially isolated, elderly individuals will often feel lonely and depressed and as a result of that may be less physically active and more prone to falls.
Living in a care home will often help alleviate many of those feeling of isolation and a care home worker will play an enormous part in that.
Having a job in which you can claim to provide both physical and (perhaps more importantly) emotional support on an ongoing, day to day basis to someone is no small thing.
Giving Somebody Back Their Dignity And Independence
If you’re anything like us you’ll probably take the ability to complete ordinary daily tasks like getting out of bed, going to the toilet or making a cup of tea for granted. For many elderly people however these tasks can be a daily struggle.
Working in a care home isn’t just about doing these jobs for someone but rather, where possible, helping them do those jobs for themselves; maintaining an individual’s dignity and independence for as long as possible.
Professional Development
A career in a care home will offer many opportunities for professional growth as well as the ability to choose to specialise your skill sets. Most care homes will support an environment that nurtures staff development with many paths open to those looking to specialise in a certain direction.
Getting To Know Your Residents
By its very nature a care home will have long term residents opposed to, say, a hospital ward or maybe even community visits where you’ll see an ever changing blur of faces.
This means that anyone who chooses to work in a care home will be able to really get to know their residents and form deep bonds with them, something most of our respondee’s said was one if not the, most rewarding part of the job.
Do you work in a care home or have you done so in the past?
What did you find to be the most rewarding part of the job? Let us know below…



