Mangar Health at The OT Show 2016

Last week the Mangar Health team exhibited at The OT Show, held at the NEC in Birmingham.
The OT Show is the UK’s largest education and trade event for occupational therapists and with over 4,500 OT’s attending every year, we thought it would be the perfect opportunity to catch up with some of our existing customers as well as meet some new friendly faces.

The Mangar Health Stand
Lauren, Daniel and Peter – our Area Representatives – were at hand for the two days, handing out cupcakes and demonstrating both new and existing Mangar products to professionals. The exhibition stand featured the Camel, ELK, Bathing Cushion and the new Ekamove – an automated patient turning device that helps prevent and treat pressure wounds.
The OT Show also saw the launch of our newly designed exhibition stand, complete with a profiling bed and a fully equipped bath to help demonstrate the Ekamove and Bathing Cushion. We received a lot of comments on how impressive our stand looked and how valuable it was to be able to experience the products in real life situations.

Speaker Session with Melanie Sturnam
There were several different speakers and CPD training sessions taking place across the two days, one of which was hosted by Melanie Sturnam, the Moving and Handling Consultant for Norfolk County Council, speaking on behalf of Mangar Health.
The session focused on Dignified Moving and Handling for People Living with Dementia and covered some important points.
Melanie started by going through a number of different considerations you should take into account when someone living with dementia has fallen, including:
- Do they need to be moved immediately?
- Are they compliant and cooperative?
- Do they have hearing or vision problems?
- Are there are any language barriers?
- Where did they fall?
- Are there any obstacles in the way?
- Are they hurt or do they need medical attention?
- Does the patient have upper body strength?
She then went on to discuss the different levels of experience people that may need to carry out dignified moving and handling may have, using a scale of 1-5. These levels were then used alongside the considerations above to advise what manual handling techniques could be used in a variety of different situations. This included the One Chair Lifting Technique, the Two Chair Lifting Technique, the Mangar ELK Lifting Cushion, the Mangar Camel Lifting Cushion and Hoists.
It was great to have attended the OT Show again this year, performing lots of product demonstrations and receiving very positive feedback. If you came to see us and would like to discuss the day in more detail; or if you didn’t attend and you would like more information on our products, please do not hesitate to get in touch. You can do this by calling our sales team on 0800 2800 485 or by emailing sales@mangar.co.uk.
Coping with Memory Loss

Progressive memory loss due to diseases like Dementia can be difficult to cope with for both someone living with the disease and their carer. With over 40% of people over the age of 65 experiencing memory loss [1], they can often need help when it comes to support and guidance.
Here are the topics covered in this article:
- What are the causes of memory loss? We have listed the most common known factors that can cause memory loss.
- Can memory loss be prevented? With the fear of memory loss at an all-time high the prevention of memory loss is widely talked about in the healthcare industry.
- Mild Cognitive Impairment. Although someone may be experiencing difficulties with memory loss it may not be server enough to be considered dementia – instead it may be Mild Cognitive Impairment.
- Memory Loss and Dementia. Dementia is often confused with Alzheimer’s, however, it is an umbrella term used to describe the symptoms that occur when the brain is affected by certain diseases – including memory loss.
- Ten Signs of Memory Loss. There are ten early warning signs to look out for if you think that you – or someone close to you – could be suffering from Dementia.
- Coping with Memory Loss. There are lots of different approaches to coping with memory loss, including the following things you can do to help aid your day-to-day life.
- Supporting someone with Memory Loss. It can be hard for someone with living with memory loss to look after themselves so we’ve listed ways in which you can help support them mentally and physically.
What are the Causes of Memory Loss?
Many of the causes of memory loss are treatable if they are diagnosed early, however, if they are not diagnosed they may progress and make treatment more difficult [2]. Research shows that there are many known factors that can cause memory loss, including the following:
- Severe sleep deprivation
- Experiencing emotional trauma
- Vitamin B-12 deficiency
- Lack of oxygen to the brain
- Excessive use of alcohol and drugs, including smoking
- Some prescription medication including antidepressants and sleeping pills
- Mental disorders such as depression, bipolar disorder and schizophrenia
- Anaesthesia from recent surgery
- Parkinson’s
- Suffering from a head injury or concussion
- Thyroid problems
- Migraines
- Having electroconvulsive therapy
- Going through brain or heart bypass surgery
- A nutritional deficiency
- A physical illness, such as a chest or urine infection
- High blood pressure and high cholesterol
Can Memory Loss be Prevented?
The fear of memory loss is something that stops many people going to the doctors for a diagnosis, with 56% of people putting off seeking a dementia diagnosis [8]. With the fear of getting dementia at an all time high one of the most talked about topics in memory loss studies is ‘can memory loss be prevented?’.
Some of the causes of memory loss that are listed above are definitely treatable, but are they preventable?
Studies show that memory loss can be prevented if you follow a couple of simple rules from a young age, to help keep your brain active and sharp.
A couple of the recommended ways to help improve your memory include going on regular walks, maintaining a healthy diet, engaging in activities that test your brain, staying social, getting a better night’s sleep, avoiding smoking and other forms of nicotine, dedicating time to relax, attending regular check-ups and using memory tests [3]. These recommendations will not prevent memory loss alone, particularly if it is age-related, however they will help improve the way in which the brain works.
Mild Cognitive Impairment
Sometimes people may notice that they are experiencing problems with their memory, however, these difficulties may not significantly affect the person’s everyday life and may not be severe enough to be considered Dementia – this is called Mild Cognitive Impairment (MCI).
It is estimated that between 5-20% of people aged over 65 are living with MCI, and 10 out of every 100 will go on to develop Dementia each year [4].

Memory Loss and Dementia
Dementia is an umbrella term and describes the symptoms that occur when the brain is affected by certain diseases or conditions. There are many different types of dementia, however some are more common than others, including Alzheimer’s disease, Vascular dementia, dementia with Lewy bodies, Frontotemporal dementia and Creutzfeldt-Jakob disease.
Alzheimer’s disease is the most common cause of dementia, named after the doctor Alois Alzheimer, who first described it as a progressive physical disease that affects the brain.
Memory loss is considered one of the first signs of Dementia and in particular, Alzheimer’s disease. In the early stages of the disease, it may be easy to mistake memory loss or lapses in judgement for the normal forgetfulness of old age, however, it will soon become apparent that the problems are becoming more severe and persistent; this is often more apparent to family and friends than to the person themselves.
Although someone may be living with memory loss, they may be able to retain certain skills for much longer. This means that they might remember a surprising range of facts or experiences, especially memories from earlier on in their life. This is because a person’s emotional memory is affected much later on in Dementia and they will still be able to remember how they felt at a particular moment in time, even if they can’t remember the specific details about it.
The extent of memory loss for someone living with the Dementia may result in difficulties carrying out day-to-day activities, as it is often caused due to damage to the hippocampus, a part of the brain that plays a very important role in day-to-day memory [5].
Ten Signs of Memory Loss
If you think you – or someone close to you – may be experiencing symptoms of memory loss and think there is a possibility it could be Dementia rather than MCI, there are 10 early warning signs and symptoms you can look out for [6].
-
Memory loss that disrupts daily life such as loss of direction
The most common sign of Dementia is memory loss, particularly when it comes to remembering newly learned information or conversations. This could mean that people lose their sense of direction and may not know where they are. Other things that may be forgotten include faces, dates, events, names, appointments, where things are stored and when to take medication.
-
Challenges in planning or solving problems
Some people may notice changes in their ability to develop or follow plans, especially if it means working with numbers. This could mean they have difficulty remembering and following a favourite recipe or keeping track of monthly bills.
-
Difficulty completing familiar tasks at home, work or in leisure
Another key early warning sign for Dementia is that people often find it hard to complete daily tasks. This could include driving to a familiar location, remembering the rules to a game or managing a budget at work.
-
Confusion with time or place
People living with Dementia can often lose track of dates, seasons and the concept of time. This could mean they have difficulty understanding daily tasks and may forget where they are or how they got there.
-
Trouble understanding visual images, spatial relationships and difficulty balancing
Vision problems are a key sign of memory loss. People may have difficulty remembering how to read, determining colour and contrast and judging distance – which may cause problems when driving. They may lose their balance and other key motor skills, meaning they have the propensity to fall over more often and may require safe patient lifting aids such as the Mangar Camel.
-
New problems with words in speaking or writing
Having trouble joining in with conversations is a major warning sign when it comes to memory loss. They may stop in the middle of a conversation and forget how to continue, possibly repeating themselves as they try.
-
Misplacing things and losing the ability to retrace steps
Someone with Dementia may put things in unusual places and forget where they are, unable to retrace their steps to find them again.
-
Decreased or poor judgment
Another early warning sign could be people experiencing changes in judgement and decision-making. For example, they could use poor judgement when dealing with money and could end up giving large amounts to sales people or canvassers.
-
Withdrawal from work or social activities
A person living with dementia may want to remove themselves from their usual hobbies, social events or work projects. They may experience trouble keeping up with their favourite sports team or avoid being social because of the changes they are experiencing.
-
Changes in mood and personality
The personality of someone dealing with memory loss can change dramatically. They may become confused, fearful, depressed or anxious. The changes they experience could easily upset them while they are at home, work, with friends or in places where they are not familiar with their surroundings.
Coping with Memory Loss
There are lots of different approaches to coping with memory loss and the feelings it can cause, such as frustration and a loss of confidence and self-esteem. Some of the techniques may require professional input from Occupational Therapists or Psychologists, however, there are lots of different things you can do to help aid your day-to-day life [7].
- Give yourself plenty of time and keep calm when carrying out tasks you feel are difficult.
- Stick to a routine where possible. Keep everyday items such as your keys and wallet in the same place and try to do tasks in the same order.
- Write any important information down and keep a pen and paper in key areas, such as next to the telephone.
- Take a shopping list with you when you go shopping and cross things off as you put them in your shopping trolley. Do the same thing at home and keep a list of things you run out of.
- Give or throw away odds and ends that are no longer in use.
- If you have trouble remembering to take items with you when you leave the house, write a big reminder note and stick it on the inside of your front door.
- Use a day-to-day calendar and cross off a day every time you go to bed, that way you will know what day is when you wake up.
- Keep a diary at home to remind you to do certain things. This could double up as a journal where you can look back and remember what you have done.
- Programme any important phone numbers into your phone so you only have to press one button to dial.
- Do deep breathing exercises to help yourself relax and stay calm.
- Use sticky notes to remind you when to do certain things, for example, when to take a book back to the library. Once you have completed the task throw the sticky note away so you don’t repeat it.
- Keep items that are alike in one place, for example, keep all of your keys on just one keyring.
- Try to focus on doing just one thing at a time, then repeat and give yourself time to learn it. If it helps, break tasks down into smaller steps.
- Talk to friends and family about how you feel and what you can do to work together.
- Use an alarm to help you to remember to do something at a particular time, such as taking something out of the oven, taking medication or making a phone call. Write down your reason for setting the alarm on a piece of paper nearby, so you don’t forget.
- Repeat important information back to someone if you need to remember it. This will increase your chances of remembering and check that you have heard it correctly.
- Try picturing yourself doing certain tasks if you can’t remember how to do them. For example, if you need to remember a recipe try picturing yourself making it and what ingredients you would use.
- Ensure you have looked into the correct equipment needed to support someone living with dementia, this could be small assistive technologies that help with household tasks, aids that help with washing and bathing, aids that help with walking and moving and adaptations to the home.
Supporting Someone With Memory Loss
At times it will be hard for someone with Alzheimer’s to look after themselves, which is where you come in. You can help support them both emotionally and physically at home in some of the following ways:
- Talk about how they are feeling and offer them reassurance.
- Help them set goals and discover what works best for them.
- Reinforce approaches and strategies that they are trying.
- Support them when they are carrying out certain activities that help their memory.
- Remember that the memory loss is not their fault.
- Don’t test them by saying things like ‘do you remember who this is?’.
- Be sensitive and supportive if they need you to repeat any information they may have already told you.
- If you are worried about the person getting lost, consider ways to support them so that they can go out.
- Encourage them to see a doctor if they haven’t already.
- Make sure there are familiar items in their home, for example, ornaments and family photographs.
- Use a notice board to display appointment cards. This should be where they will clearly see it.
- Try not to show the person that you are upset by them not remembering your name or recognising you.
If you notice any of the 10 warning signs in either yourself or someone you know it is advised that you schedule an appointment with your doctor so they can assess your needs. If you need additional support or information on coping with memory loss the NHS has a range of useful documents and contacts.
To find out how Mangar can help please contact us.
[1] http://www.nhs.uk/Conditions/memory-loss/Pages/Introduction.aspx
[2] http://www.healthline.com/symptom/memory-loss
[3] http://www.webmd.com/healthy-aging/features/9-brain-boosters-to-prevent-memory-loss?page=2
[4] http://www.rcpsych.ac.uk/healthadvice/problemsdisorders/dementiaandmemoryproblems.aspx
[5] https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=123
[6] http://www.alz.org/10-signs-symptoms-alzheimers-dementia.asp
[7] http://www.brainandspine.org.uk/memory-problems-and-tips-how-cope-them
[8] https://www.alzheimers.org.uk/site/scripts/news_article.php?newsID=2606
The Cost of Pressure Ulcers

“The cost of pressure ulcers to the NHS are estimated to be £1.4 – £2.2 billion annually, making pressure ulcers the single most costly chronic wound to the NHS”
Pressure care is a daily challenge for healthcare professionals when caring for bed-bound and immobile patients. While NHS budgets are hit by austerity measures and the cost of pressure care constantly increases, experts in the field are racing to find solutions to improve healing rates and the patient experience.
As Tissue Viability Nurses across the UK educate colleagues and issue guidelines designed to prevent vulnerable patients developing wounds, they are faced with increasing demands on the service from an ageing and growing population. Nearly 7,000,000 people across all care settings will be affected by a pressure ulcer each year with predictions that by 2020 the cost of wound care for the average CCG will reach £55m. (UCLH NHS)
Very simply, pressure sores develop when a large amount of pressure is applied to an area of skin over a short period of time. The extra pressure disrupts the blood flow and the affected skin becomes starved of oxygen and nutrients, which causes it to break down and ulcers begin to form [2]. Most affected are those aged over 75 as their skin becomes thinner and frailer.

The cost of pressure ulcers to the patient
Patients who develop pressure ulcers become extremely uncomfortable and painful wounds can cause patients to have trouble sleeping, which in turn hinders recovery speed. In severe cases, pressure ulcers can result in major harm or death.
Research into pressure care over recent years has helped to educate healthcare professionals to deliver greater preventative care and improved healing rates. Opinion on the outlook for pressure care is mixed but best nursing practice and the appropriate medical equipment can certainly move patient care in the right direction.
Why does pressure care cost so much?
The cost of the healthcare professional accounts for 90% of the overall costs for treating pressure ulcers, with the remaining 10% being spent on treatment and specialist equipment [4]. With up to four people required to reposition a patient every 2 hours, you can easily see how costs for pressure ulcer care can be high.
As new, innovative equipment is developed to support Tissue Viability Nurses and Pressure Care Professionals implement pressure ulcer reduction initiatives, the standards of healing will improve. Foam and dynamic mattresses, positioning cushions and automated positioning systems such as the Ekamove, reduce the amount of manual intervention required while delivering personalised care.
The cost of treating a pressure ulcer varies between £1,064 to £10,551 depending on the Grade [6]. The costs increase with ulcer grade for a number of different reasons including the time taken to heal and the likelihood of complications in the most severe of cases. For severe cases where surgery is required the cost could be up to £14,000 [7].

Pressure care in the community
Pressure wounds are not just a hospital or care home challenge. As people are discharged to their homes, their care will often fall to loved ones. These ‘unpaid carers’ are doing so against a backdrop of cuts to social security and local care services. This is not only unacceptable but dangerously unsustainable. If carers aren’t supported to care well for both themselves and their loved ones, the NHS and other public services would be forced to step in. With NHS and local authority budgets already stretched to their limits, this would bring them to their knees. (Care UK)
Stop the Pressure
With the cost of pressure ulcers to the NHS continually rising people are becoming more and more concerned with how they can be prevented. Over the last few years, a ‘Stop the Pressure’ SSKIN campaign has been launched to help raise awareness to those that may not already know the warning signs and indicators, giving them a detailed guide to follow when caring for all vulnerable patients.
SSKIN is a five-step model for pressure ulcer prevention [8] and includes the following:
- Surface: Make sure patients have the correct support
- Skin inspection: early inspections mean early detection
- Keep patients moving
- Incontinence/moisture: make sure your patients are always clean and dry
- Nutrition/hydration: give patients a healthy diet and plenty of fluids
4% of the NHS budget is currently attributed to pressure care with all forecasts predicting an increase in line with a growing, ageing demographic. Priority must be given to the prevention and fast healing of pressure wounds, using education and technology to reduce the pressure on patients, healthcare professionals and the NHS alike.
To find out how Mangar Health can help assist you with pressure care prevention please contact us here.
[1] https://www.england.nhs.uk/2014/01/stop-the-pressure/
[2] http://www.nhs.uk/conditions/pressure-ulcers/pages/introduction.aspx
[3] https://www.england.nhs.uk/2014/01/stop-the-pressure/
[4] https://www.nice.org.uk/guidance/cg179/resources/costing-statement-24868810
[5] http://content.digital.nhs.uk/catalogue/PUB17903
[7] http://ageing.oxfordjournals.org/content/33/3/230.abstract
[8] http://harmfreecare.org/2012/04/nhsmideast-stopthepressure/
The Prevention of Pressure Ulcers

The prevention of pressure ulcers and bedsores is a widely discussed topic in the healthcare industry, particularly among those working in hospitals, care homes or looking after people in their own homes.
There are four stages [1] to pressure wounds, however, research has proven that 95% of pressure ulcers in patients are preventable [2] before they reach the first stage, which would save the NHS almost £3.8million in costs per day.
The Stages of Pressure Ulcers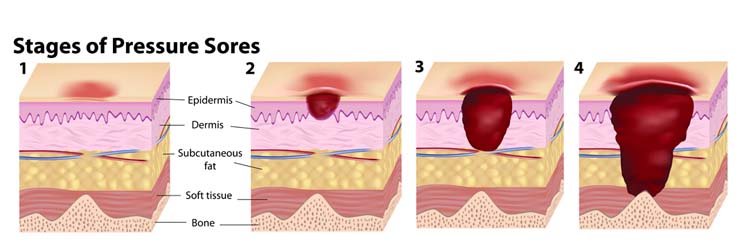
Stage One
Stage one is when the skin is not broken, but there is a sign of hardened, heated and discoloured skin. If pressed the wound remains red and does not lighten or turn white, and after 30 minutes the change in colour does not fade.
Stage Two
A stage two pressure ulcer is when the top layer of skin is broken, creating a shallow open sore. The second layer of skin may also be broken and there may be signs of drainage or fluid leakage.
Stage Three
Stage three pressure wounds extend through the second layer of skin into the subcutaneous tissue below. Although bone, tendon, and muscle are not visible at this stage there may be signs of pus, odor, fever and a greenish coloured drainage.
Stage Four
A stage four ulcer is when the wound has extended as far as the muscle or bone. There will be a lot of dead tissue and drainage present, increasing the risk of infection.
How can they be Prevented?
Pressure ulcers are likely to develop when there is too much pressure on the skin for long periods of time, which often happens with bedridden patients. Not only do they cause pain and discomfort, but stage three and four sores may lead to infections such as meningitis and cellulitis [3], which is why preventing them is so crucial to healthcare professionals and caregivers.
If you or someone in your care is currently on bed rest, there are several things you can do to help prevent pressure ulcers forming.
Changing Position
To reduce the amount of pressure that is applied to your skin over long periods of time it is important that you change your position regularly. It is recommended that people who are confined to bed should change their position at least once every two hours.
If you are unable to change position for yourself a carer or relative will need to assist you, or if you don’t have someone available to turn you regularly there are automatic patient turning systems, such as the Ekamove patient turning system.
Checking your Skin
To help identify the possibility of a pressure wound forming it is crucial to check your skin for warning signs several times a day. It is important to pay attention to problem areas, including your heels, ankles, hips, spine, elbows, shoulders, tailbone, ears and the back of your head.
If you can’t see certain areas of your body easily use a mirror or ask a caregiver to look.
Nutrition
Maintaining a healthy and balanced diet [4] that contains enough protein, vitamins and minerals can help minimise the risk of skin damage to bedridden patients. You may be referred to a dietitian so that an appropriate plan can be drawn up for you, however, the following is recommended to everyone:
- Eat small, regular meals rather than two or three larger meals. If you set a timetable that details when you should eat and don’t wait until you’re hungry, it can help to ensure you receive the necessary nutrition throughout the day.
- Avoid drinking large amounts of fluid just before as meal as it makes you feel fuller than you actually are.
- If swallowing is difficult, try drinking soups, specially made drinks or pureed foods.
- If you’re a vegetarian eat high protein alternatives to meat. This could include cheese, peanut butter, yoghurt, custard and nuts.
Using Pillows or Cushions
Another effective way of preventing pressure ulcers is to put pillows between the parts of your body that will press against each other, such as your shoulders, elbows, knees and ankles.
There are also specialist cushions and pads available that can help relieve pressure for bedridden patients, including mattresses, overlays and heel cushions [5].
Staying Clean and Dry
The cleaner and drier your skin is, the less likely it is you will develop pressure ulcers. Dip a washcloth in a tub of warm water and mild soap to clean your skin with it on a daily basis, lightly patting your skin dry with a towel. Make sure not to rub the skin or massage any treatments into it as it can lead to mild skin irritation.
If you’re worried about either you or someone in your care developing pressure wounds please speak to your healthcare professional. However, if you would like more information on pressure care and preventing pressure ulcers from Mangar, please get in touch to find out how we can help.
References
[1] http://www.msktc.org/sci/factsheets/skincare/Recognizing-and-Treating-Pressure-Sores
[2] http://nhs.stopthepressure.co.uk/Learning/index.htm
[3] http://www.advancedtissue.com/5-tips-for-preventing-bed-sores-in-bedridden-patients/
[4] http://www.nhs.uk/Conditions/Pressure-ulcers/Pages/Prevention.aspx
[5] https://www.drugs.com/cg/how-to-prevent-pressure-ulcers.html
New Mangar Health Websites Launched!

After months of teaser Tweets on the Mangar Health Twitter, we are delighted to announce the launch of the new Mangar Health Websites. To help make your Mangar Health experience better, no matter where you are in the world, we now have individual websites to target our Global, UK, American and German markets.
The new sites are designed to make it easier for you to find the information you are looking for, with specific pages that target our client sectors.
The new easy-to-navigate stores are now separated into four product sectors – patient lifting, bathing, bed and accessories, making it easier for you to shop for the products you need.
As well as the updated stores we now have our ‘Knowledge’ centre. This will regularly be updated with news, case studies, videos and resources for you to download.
The sites are fully responsive, meaning they can easily be used and are accessible on any device.
Please take a moment to have a look around our new sites – we hope you like the new and improved look. Feel free to contact us with any comments.
A Day in the Life of a Mangar Health Territory Account Manager

Last Friday our new Marketing Executive, Kirsty, went out with John Finister, the Territory Account Manager for Wales and Central England.
As it was her first week at Mangar Health the aim was for Kirsty to see what it’s like to spend a day in a Territory Account Manager’s life and experience the value of Mangar products first hand, so John took her to several of his appointments across Coventry and Leicester.
A day in the Life of a Mangar Health Territory Account Manager
08:20am – I arrived in the Birmingham area to meet Wales and Central England Territory Account Manger, John Finister.
John introduced himself and said he has been in the healthcare industry for just over 10 years, starting as Area Manager at mobility retailer Keep Able, in 2006. Six years later he moved on to work at Betterlife as a Trainer, finally joining Mangar to manage Wales, Central and Eastern England in April 2013.
He added that he loves working at Mangar and enjoys that he can provide practical and simple solutions that allow people to have a dignified and independent everyday lifestyle. His favourite aspect of his role is the rewarding feeling he gets knowing he has left his client in a better way than when he first met them, and that as a company Mangar meets their challenging targets by satisfying the increasing demand for solutions.
We talked through the plan for the day and John mentioned that as every day is unpredictable for a Territory Account Manager, it was all subject to change as we got on the road.
The plan for the day was to go to Coventry for an ELK demonstration with an Occupational Therapist, then onto Leicester to meet an OT for two separate appointments. The first appointment was to offer additional support to a client with a Mangar Leg Lifter, and the second was to demonstrate a Handy Pillow Lift.
While we chatted through the day’s itinerary John received a couple of calls asking for some of his appointments to be changed, something he said happens a lot.
09:30am – The first stop of the day was the Coventry Opal Centre.
John showed me round The Opal Assessment and Demonstration Centre, a place for people who need help to live at home. The demonstration centre had a fully fitted bathroom, bedroom, living room and kitchen that featured the different types of equipment people may need to assist them with everyday living. This included bathing equipment, chairs, beds and a range of small aids.
For me, looking at the Mobility Assistance and aids that are available was really helpful. John gave a great explanation as to why these centres are so useful to both OT’s and clients, as it allows them to physically look at all of the options available to them in ‘real-life’ situations. He showed me the Mangar equipment that was already in place and gave examples of different scenarios in which people may need to use it.
After our quick look around, we headed to our first OT appointment in Coventry.
11:00am – John’s first appointment of the day was a home visit with a local Occupational Therapist. We met the OT outside just before 11:00am to talk through her client’s case and discuss anything that the OT thought might be important. The first thing the OT highlighted was that the main aim of this meeting was to protect the carer, as she had been struggling to lift the client after he’d fallen.
We found out that the client was a wheelchair user who had been experiencing a lot of falls moving from both the car and bed back into his wheelchair. His fiancé had been finding it challenging lifting him from the floor, so John was there to look at how she is currently doing it and discuss the options that are available to her for a safer lift, in particular, the Mangar ELK Cushion.
John and the OT carried out a demonstration for the client, making sure his fiancé knew how to inflate and deflate each section of the ELK cushion. Once they had inflated the cushion with the Occupational Therapist demonstrating, John asked the client if he’d like to try the cushion out for himself.
As the cushion was already inflated, the Client moved from his wheelchair to the bed and then onto the Mangar ELK. Once he had let John and the OT know he was happy sitting on it, his fiancé deflated the sections one by one. John pointed out that they wouldn’t have to do this process again as there would never be a need to lower him to the ground. The important part was seeing if it was easier for his fiancé to raise him back up to a level where he could reach his wheelchair.
The demonstration and test went really well and after all questions had been answered John and I left the OT with the client to go through the next steps of the process.
12:30pm – We made a quick stop at ASDA to pick up some lunch and while eating, John explained that the next visit was to see a client he had been to before for aMangar Leg Lifter.
The client was suffering from both a heart condition and COPD and had been struggling to lift his legs into bed without help, so he had a Leg Lifter to help him get into bed without the assistance of a carer. The client felt he needed a little extra assistance using the Leg Lifter and had asked John for some additional support and guidance.
1:30pm – Once inside John and the Occupational Therapist showed the client the best way to use the Leg Lifter, which made me see the full value of the product. By the end of the appointment, the client’s confidence had lifted and he mentioned how much he felt the Leg Lifter was going to help his independence.
2:00pm – Our next appointment was scheduled for 3.00pm on the other side of Leicester and as soon as John had finished fixing the Leg Lifter we headed out. First, we met with the OT again for a quick catch up.
3.30pm – Our 3.30pm appointment was for a client that had been experiencing muscle spasms that made it very difficult for him to sit up or walk. It has not yet been diagnosed by doctors, however, the OT was visiting to see if one of ourMangar Handy Pillow Lifts would help him sit up in bed and get into a position where he can get out of bed without any assistance.
The client had previously been using a bed lift which meant that when he wanted to raise himself up he had to lift the whole mattress, which he found difficult to use.
When we arrived John demonstrated the Handy Pillow Lift, getting the client to test it as he went along. As the client struggled to lie on hard surfaces, he thought the fact the Pillow Lift was soft enough to mold to his shape was perfect for him and he was extremely grateful we were able to offer such a simple solution to a problem he has been experiencing for so long.
If any Occupational Therapists would like to see the Clinical Business Case for the Handy Pillow Lift, you can find it here.
4:00pm – John’s 4:00pm appointment for a Mangar Bathing Cushion was cancelled by the OT, so it was time to head home.
5:30pm – After a long drive back home to Telford, my eventful and interesting day finished at 5.30pm.
Before I left John mentioned that a busy day on the road is not the end of his day-to-day job, as when he gets home he then has to reply to emails, organise his quotes from the day, respond to voicemails, make new appointments and fill out any necessary paperwork. I’ve definitely realised that the Territory Sales Team don’t have a standard 9-5 job, especially as sometimes work can overflow into the weekend.
It was great to experience a day on the road with John and it has really given me some insight into the positive impact our lifting products can have on people’s lives.
If you’re in the Wales and Central England area and would like to talk to John about Mangar and some of our products you can call him on 07909 536426 or email jfinister@mangar.co.uk. If you’re in other areas you can find your nearest representative here.
Travelling with a Bath Lifter

As the summer holiday season approaches thoughts will inevitably turn to the logistics of packing for our relaxing time away. For those of us who holiday in the UK, the main logistical issue will be ensuring we have all items of clothing to deal with the range of weather conditions we are likely to have thrown at us. However, the logistics of packing becomes far more complicated for older and disabled people who have the additional challenges of deciding what equipment they might need to take on holiday so that they can enjoy the relaxing benefits of going away on holiday.
Travelling with a Bath Lifter
Over the past few years travel guides, holiday accommodation websites and brochures have begun to improve the accessibility information provided on places to visit and to stay. With this information, older and disabled people are able to make an informed decision on where they can experience a relaxing holiday. Understandably, people want to take their own equipment, such as bath lifters, on holiday. Familiarity with the way their own equipment works, or what the condition of any equipment provided by holiday agents will be in on arrival, reduces the worry of having no equipment or relying on loaned piece of equipment.
Sadly, as social services occupational therapists I was seldom in the position where my professional reasoning extended beyond the usability of bathing equipment in the home. Thankfully, this soon changed when I moved into independent practice. In this new role, I had to provide advice and recommendation to people who wanted to be able to take bathing equipment on holiday. This requirement to take equipment on holiday has added a whole new dimension to my professional reasoning.
Through this experience, I have following tips about taking bathing equipment on holiday. Firstly, the bathing equipment can’t be bulky or heavy. People will not travel with bathing equipment that takes up valuable room for luggage and other holiday paraphernalia.
People also want to avoid having to lug a heavy piece of equipment from the car to the accommodation. As well as this, the equipment needs to be discreet. This is a tricky one because wanting to hide the use of equipment feeds into the medical model of disability, and why should people feel embarrassed about having to use equipment. However, in my experience people want to have the choice about this and having something that doesn’t stick out like a sore thumb as you unpack the car is an important consideration for many of us.
Finally, I have learnt that the equipment has to be able to fit into the bath. This point may seem obvious, but the design of the bath at home is unlikely to be the same as the one on holiday. Therefore, it is important that the bath lifter is easy to adjust and has the flexibility in design to accommodate a wider range of bath shapes, materials, and depths.
Whilst very few of the bath lifters on the market can achieve all of the requirements I have just highlighted above the Mangar Bath Cushion comes close. Being lightweight, extremely portable, and having the type of powerful suction feet that fits most bath surfaces, the bath cushion offers the discreet and flexible bathing solution people want when they go on holiday. As occupational therapists, we know that holidays contribute to the health and well-being of the people we work with. Whilst there may be funding issues around the choice of equipment we recommend, it is still important we consider how the choice of bathing equipment will influence what older and disabled people will have to pack when they go on holiday.
Mangar International at NAEP National Annual Conference 2016

Mangar International are exhibiting at the National Annual Conference 2016 taking place at the Chesford Grange Conference Centre and Hotel, Warwick on the 14 and 15 June 2016. You can find us on stand 19.
There is still time to book your place this year’s NAEP National Annual Conference. Esteemed speakers and presenters from the healthcare and associated sectors we will be aiming to help you unravel the mysteries of the Care Act and what it all means in relation to both the health and social care sectors.
The conference aims to provide you with the insight to enable the better use of your resources in the face of ever rising demand, the guidance to provide a seamless health and social care service to the public, combined with an intuitive understanding of the relevant legal elements of the Act.
Speakers include:
- Roy Lilley
- Rt Hon Paul Burstow
- Michael Mandelstam
- Dave Thompson, MBE DL, Chief Executive, Warrington Disability Partnership
- Denise Cross, Professional Manager of Occupational Therapy & Wheelchair Services, South Warwickshire Foundation Trust
- Rachael Mathers Senior Occupational Therapist, South Warwickshire Foundation Trust
- Wendy Meredith, Director of Population Health Transformation, Greater Manchester Health and Social Care Devolution Team
Topics include:
- Unravelling the Mysteries of the Care Act – A Topical Look at the Sector Today
- The Health and Social Care Act (Early intervention, clinical assessments, prescribers, personal budgets and includes case studies)
- Care Act One Year Old: Baby Steps, Big Challenges
- Community Equipment Policies And Practice: The Good, The Bad And The Law – Michael Mandelstam
- Health and Wellbeing – Wendy Meredith, Director of Population Health
- First Class Delivery: Integration at What Cost?
- The ‘ABC…and D!’ of 7 Day Working – Developing an Overarching Service Model
- To Reposition or Not To Reposition? That Is The Question
- Root Cause Analysis
- In House Services in a Competitive World
- Savings on Equipment Provision
- Regulatory, Cross Border Arrangements and Unable To Obtain Access Issues
- Roles and Responsibilities in the Prescription of Equipment
- Dementia, Falls and Prevention
- The Better Care Fund
To view the Conference Programme please click on the following link: 2016 Conference Programme.
New CEO of Mangar International appointed

Mangar International has named Simon Claridge as its new CEO.
Established more than three decades ago, Mangar International is a UK healthcare company, with customers across Europe and North America. Investment by YFM Equity Partners in 2014 has enabled the company to create a robust business strategy and Simon’s appointment as CEO is critical to the successful delivery of the ambitious growth targets.
Mangar Chairman, James Buckley said: “I am pleased to be welcoming Simon to Mangar International and look forward to him building on the recent successes we have enjoyed. He brings a wealth of experience leading teams and achieving strategic goals. We are thrilled to have him.”
With a successful track record in developing business growth and change management, Simon has spent the last 3 years as Vice President of UK Sales for medical device company ArjoHuntleigh. Previous to that, he spent 5 years with leading pharmaceutical company GlaxoSmithKline.
Simon said: “I’m delighted to be joining Mangar International and I’m looking forward to the challenge of implementing the new business strategy. In the short time since I arrived, I’ve been pleased to find such a motivated team of staff who are committed to business success.
“The Mangar product portfolio of inflatable moving and handling equipment is unique and already valued by healthcare professionals globally. I feel privileged to be leading the company’s business growth at such an exciting time.”
Simon, 41 lives in Cambridge with his wife and three daughters.
For more information contact Clare Birt
Email: cbirt@mangar.co.uk
M: +44(0)7977 576646
T: +44(0) 1544 267674
Welsh and English Care Acts

Introduction
In England, occupational therapists working in adult health and social care are experiencing subtle, yet transformational, changes to their role. Arguably, these changes are as a consequence of the Care Act and the impact it has had on the delivery of services since its implementation in 2014.
Soon, colleagues in Wales will also have the opportunity to experience the transformational effect changes to health and social care legislation brings, as the Welsh version of the Care Act comes into force. In this blog, we take a brief look at similarities and differences between the two acts.
Health and social provision
Whether you an OT in England or in Wales, you will both be looking at health and social provision in terms of how older and disabled people and their carers can be supported to maintain a sense of well-being. Also similar is the process older and disabled people have to negotiate in order to receive support.
The process starts with an assessment, which considers what the person or carers needs or wants to do in order they can maintain their well-being. Once this has been established, a person, or their carer, receives advice or information as to the ways in which maintaining their health and well-being can be achieved. Social care services will provide service, or direct payments if any support meets the national eligibility criteria for the provision of care.
Finally, but no less important, is the focus on prevention. In order to prevent people developing needs, both the Welsh and the English Act are placing an emphasis on encouraging the development of preventative services. And this is where the expertise of occupational therapists plays, and will play, an important role. For it is the skills and knowledge the profession has on re-ablement, equipment, adaptation, and the use of advice/education to improve independence and safety will play a vital role in delivering these services.
So what are the key differences between the Acts in England and Wales?
The health and social care needs of children is one of the biggest differences, with children being considered in the Welsh Act but not in the English Act, which will remove the often difficult time during the transition period from child to an adult. The Welsh Act has also placed a greater emphasis on safeguarding as demonstrated by the adult protection and support order tools they have put in place a national safeguarding board, which will have a role in supporting local boards.
Finally, the Welsh Government is taking the opportunity of legislation change to motivate the NHS and social care departments to continue with moving forward with integration agenda. It is doing this by giving itself the power in the Act, if necessary, to force partnership agreements between the local NHS and local authority departments.
The key differences are, therefore,
- The Welsh Act includes children
- Improved safeguarding procedures
- A stronger push towards health and social care integration
Conclusion
Over the coming months and years, it will be interesting to watch whether the differences in the Welsh Care Act makes it a stronger piece of legislation when compared to its cousin act in England. Only time will tell if this is the case. In the meantime, if you are an OT and want to know about how the Welsh act will impact on practice, you can visit http://gov.wales/docs/dhss/publications/151217occupationaltherapyleafleten.pdf.
And remember, if you are a member of College of Occupational Therapy, then you will find an English and Welsh language version of their position statement on the act https://www.cot.co.uk/position-statements/position-statements
Crisis Response Falls Team: Reducing Admissions and Repeat Falls

Provided by:
East Midlands Ambulance Service NHS Trust
Published by:
The following case study provided by East Midlands Ambulance Service NHS Trust describes how a demand for better falls service was effectively provided by integrated health and social services providers. The emergency lifting equipment referred to throughout the case study are Mangar ELK and Camel lifting cushions.
Details of the initiative
Falls-related calls make up about 20% of all calls received by the East Midlands Ambulance Service (EMAS); approximately 90,000 calls per year. Reducing demand on hospitals and the potential negative outcomes associated with hospital admission for patients and psychological impacts are important priorities.
EMAS covers several counties with a combined population of 4.8 million. The solution developed in the Northamptonshire area (population 700,000) is the Crisis Response Falls Team (CRFT). The CRFT comprises specialist ambulance crews and a social care support team.
The ambulance crews include 7 staff made up of paramedics and emergency care assistants who are trained in enhanced diagnosis and lifting techniques related to falls. The ambulance control’s computer system uses an algorithm to dispatch a CRFT ambulance to people who have fallen. The crews use 2 bariatric ambulances and specialist lifting equipment to ensure people of any size who fall can be helped.
Enhanced diagnosis and faster access to lifting equipment helps to reduce conveyance to the hospital and subsequent admissions. The service prior to the inception of the CRFT was a standard ambulance response, often requiring either a manual lift of a person who has fallen or a further response with appropriate equipment. In both cases, a person who had fallen may have been left in situ for a significant period of time, causing secondary injuries, exacerbating primary injuries and potentially reducing the quality of life or life expectancy.
The CRFT social care support team is provided by Northamptonshire County Council, under a contract with a social care provider. The social care team works with people who have fallen, who are referred by the CRFT ambulance crews, other clinicians or the local authority. The social care team is able to assess people in their own home and identify risk factors for repeat falls, remove trip hazards and install aids to help reduce the risk of repeat falls. They also attend A&E to assess patients and facilitate discharge, undertaking a home visit and supporting patients afterwards, thereby avoiding unnecessary admissions. Patients may be referred to consultant geriatricians for further assessment and support if required.
Falls are the leading cause of mortality in people aged over 75 in the UK
Falls are the leading cause of mortality resulting from injury in people aged over 75 in the UK (NHS Confederation 2012). Delayed responses can exacerbate these injuries and present secondary negative impacts for a patient. Even those that do not suffer an injury from the initial fall can still die if they are not able to call for help.
The number of people aged 60 or over in the UK is expected to reach 20 million by 2031 (NHS Confederation 2012), and the proportion of people living past 85 is also likely to increase significantly. This means falls will make up an even greater proportion of calls made to the ambulance service, placing a greater strain on frontline resources and staff. In addition to this, obesity levels in the UK are increasing.
Obese or bariatric patients may require mechanical lifting equipment to help them when they fall as manual handling techniques place staff at risk of injury. This can result in treatment delays and adds further pressure to the ambulance service. Bariatric ambulances are used as they can accommodate any size of the patient, in contrast to normal ambulances.
Savings delivered
This initiative saves money by reducing the proportion of falls related calls that result in hospital admission. From over 1300 referrals accepted by the CRFT in Northamptonshire in 2012, just over 1000 admissions were avoided. These were as a result of faster access to specialist lifting equipment, enhanced diagnosis to avoid conveyance to A&E and the support offered by the CRFT to facilitate discharge from A&E.
Based on the 2012 cost data, each referral accepted by the CRFT cost £778 and each admission avoided saved £1556. The net saving from 1,050 admissions avoided from 1,311 referrals was therefore approximately £640,000; equivalent to £91,000 per 100,000 population.
The cost of the CRFT response takes into account the additional staff required, training and the cost of the contract with the social care provider to provide support to those who fall. The additional equipment is a non-recurrent capital cost, accounted for under ‘Any costs required to achieve the savings’ below.
Avoiding unnecessary conveyance to hospital helps to avoid unnecessary admissions. The conveyance rate for people who fall attended by the CRFT is around 40% compared to 65% for those attended by a normal ambulance. This is due to the improved diagnosis and management of falls-related injuries provided by the specialist service.
This initiative is also likely to reduce the number of repeat falls due to improved assessment and management of risk factors, although it is not possible to confirm this with the available data. Whilst this saving cannot be accurately quantified and has not been included, the number of falls-related calls in Northamptonshire has stabilised at around 10,500 per year in contrast to previous annual rises, which were believed to be due to demographic changes.
Costs required to achieve savings
Change requires non-recurrent costs equivalent to less than 6 months’ savings. These costs include training CRFT ambulance crews in enhanced diagnosis and treatment of people who fall and the procurement of 2 bariatric-capable ambulances, plus lifting equipment.
EMAS in Northamptonshire was able to procure 2 ambulances second-hand for approximately £7000 each, with additional equipment costs of around £2000 per vehicle. This is a significant saving over the purchase of brand new vehicles. If new vehicles were required the cost would still be less than 1 year’s savings, however. Running costs of the vehicles have been taken into account in the cost of the CRFT response and reflected in the net savings.
Employing a dedicated falls team was considered more economical than providing specialist falls training and equipment to all ambulance crews in Northamptonshire.
Supporting evidence
In Northamptonshire, CRFT intervention either avoided a hospital admission directly by avoiding conveyance to A&E, or facilitated a discharge directly from A&E (therefore avoiding a hospital admission) in 1,206 cases. After further assessment, 156 of these patients were subsequently admitted to a hospital, giving an estimated 1,050 avoided admissions.
The cost of falls to the NHS is estimated at £2 billion per year in bed days, with hip fractures alone adding a further £2.3 billion per year (NHS Confederation 2012).
Quality outcomes delivered
There is a significant improvement in care quality as assessing, lifting and treating people who have fallen can be achieved faster and safer due to the improved training and equipment of the specialist CRFT ambulance crews. All patients who fall will benefit from the greater knowledge and capabilities of the CRFT compared to a standard ambulance response, but particularly those who would otherwise have to wait for a bariatric vehicle.
Care quality is also improved as risk factors for repeat falls are identified and managed appropriately by the CRFT after the first fall. This includes managing physical risks such as trip hazards, installing aids, or referral to a consultant geriatrician for the management of conditions that may exacerbate the risks or consequences of falls. The CRFT social care team supports approximately 1,000 people per year in Northamptonshire.
The social care support team is also able to assist the discharge of patients from A&E and avoid hospitalisation as they can quickly attend to assess patients in A&E and undertake a home visit. These patients are therefore at a lower risk of healthcare acquired infection and other hazards resulting from hospitalisation.
Impact on patients
The CRFT is able to safely lift and move patients who have fallen, who might otherwise be left in place until more specialised equipment is available. This helps to reduce exacerbation of primary injuries and prevent secondary injuries and distress resulting from being immobile on the floor. Patients who can be treated at the scene or in the community with the assistance of the social care team are at a lower risk of healthcare acquired infection.
Impact on patients, people who use services, carers, public and/or population experience
One significant impact of a fall is a fear of falling again. The identification of risk factors, advice and support given and the knowledge that specialist help is available, all help to reduce this fear and improve the quality of life.
An evaluation by the University of Northampton (Campbell 2013) found that patient feedback was positive. Key points given by patients included: building confidence, helping to maintain independent living and to stay at home, providing appropriate support and advice, and access to on-going care. The social support offered by the service was seen as a particular benefit to patients.
Evidence of deliverables from implementation
The initiative commenced in November 2011 in Northamptonshire and an independent evaluation (Campbell 2013) assessed its performance for 12 months.
During this time CRFT intervention reduced hospital admissions either by avoiding conveyance to A&E or by facilitating discharge directly from A&E, in 1,206 cases. 156 of these patients were later admitted to a hospital, giving an estimated 1,050 avoided admissions in the county (Campbell et al 2013).
During the evaluation period, the social care team received a total of 1,546 referrals. 85% of these referrals were accepted by the service. Over 40% of social care referrals originated from the CRFT falls ambulances. Almost 50% of these were made for the purpose of avoiding hospital admissions and 43% sought to aid discharge from A&E departments.
Prior to implementation, a steady rise in falls-related calls was observed, which was believed to be due to demographic changes such as the aging population. A year after implementation the number of falls-related calls has stabilised at around 10,500 per year in Northamptonshire. It is not possible to prove a causal link using the data available, but the initiative is believed to have contributed to this stabilisation by reducing the risk of repeat falls among those referred to the CRFT.
For the full report visit:
Blue Light Services Join Forces to Launch North East Emergency Medical Responder Scheme

A new six-month trial scheme will see North East Ambulance Service (NEAS) and the four Fire and Rescue Services based in the region work together to save more lives.
Demand on the Ambulance Service has increased by nearly 20 per cent since 2007. During the past ten years, firefighters nationally have been attending fewer fires, thanks to their successful programmes of community safety work. At the same time, the variety and complexity of rescue incidents firefighters respond to has broadened along with the specialist skills needed to meet these challenges. These changes in activities have resulted in demand for FRS services remaining extremely high.
The Fire and Rescue Service
The Fire and Rescue Service (FRS) is not funded to provide the response to medical emergencies, however, it is already carried out in some FRSs by employees on a voluntary basis. The trial is part of a review of the terms and conditions of firefighters by the National Joint Council for Local Authority Fire and Rescue Services, looking at the current and future demands on the service and profession.
NEAS Director, Caroline Thurlbeck said: “NEAS receives a new 999 call every 65 seconds, and in an emergency, seconds count.
“During this innovative trial, an Emergency Medical Responder (EMR) will be dispatched at the same time as an ambulance. Our ambition for this trial is to improve the survival rate for those people who suffer from http://mangar.co.uk/2016/01/13/blue-light-services-join-forces-launch-north-east-emergency-medical-responder-scheme/a life-threatening illness or injury in the community. The location of EMR’s within local communities could mean they are nearer to the scene and can deliver lifesaving care in those first critical minutes of the emergency until an ambulance clinician arrives, enhancing the usual emergency medical response from NEAS.
Evidence shows that an early intervention with a defibrillator or CPR can improve survival chances and also the quality of life for the patient afterwards.”
Latest figures show that a quarter of all cardiac arrests attended by NEAS have a return of spontaneous circulation, with just over three percent of patients surviving to be discharged from hospital.
Emergency Medical Response Units Trial
During the trial, Emergency Medical Response Units, in the form of fire appliances, will deliver emergency medical services when requested by NEAS. The emergency medical services included may involve attending calls where people are suffering from chest pain, difficulty in breathing, cardiac arrest, and unconsciousness not due to trauma.
Emergency Medical Responders have been trained to enhance their existing medical care knowledge, including basic life support by managing a patient’s airway, giving oxygen therapy, including assisted ventilation, delivering cardiopulmonary resuscitation (CPR) and defibrillation using a semi-automatic AED and controlling blood loss.
The EMR’s are equipped with a kit which includes oxygen and an automated external defibrillator (AED) to help patients in a medical emergency such as a heart attack, collapse or breathing difficulties.
Feedback
Chief Fire Officer Ian Hayton from Cleveland Fire Brigade said: “The scheme involves trained firefighters attending incidents in areas where we can reach a casualty and maintain life or reducing suffering and anxiety until a paramedic arrives. This really is a lifesaving partnership; Cleveland Fire Brigade staff can complement and work alongside the professional healthcare staff at North East Ambulance Service to improve patient care outcomes. Cleveland Fire Brigade’s ethos is to make a difference to the lives and safety of our local community. This critical partnership with NEAS allows our firefighters another opportunity to demonstrate how they can achieve that goal.”
Northumberland Fire and Rescue Service Assistant Chief Fire Officer Mark McCarty said: “We are looking forward to working in partnership with the North East Ambulance Service to provide an enhanced level of response to emergency medical incidents. Our firefighters are used to dealing with medical emergencies as part of their role and already work closely with NEAS colleagues in a number of emergency situations. In this pilot, if one of our teams is available when a medical emergency response is requested, we can be at the scene quickly to begin life-saving treatment while waiting for an ambulance crew to arrive, who will then be able to continue the treatment and provide specialist medical care. This is a great opportunity for us to use our skills and training to further benefit the whole community.”
Keith Wanley, the area manager for County Durham and Darlington Fire and Rescue Service, said: “We are extremely pleased to be involved in the regional emergency medical response trial, which will enhance the close working relationship and collaboration we have with our partner agencies. Our fire crews already save many lives through well-established home safety prevention work and by providing a professional response to a wide variety of incidents where people are trapped. From Monday, our fire crews will be expanding their response role to provide medical assistance to people with life threatening conditions, when requested by NEAS, until an ambulance crew can arrive. Also, from the end of January, they will be expanding their prevention work into a range of areas which will including advice and support to prevent trips and falls in the home and other health advice. We hope this trial will provide effective early intervention and support to save many more lives.”
Chris Lowther, Assistant Chief Fire Officer at Tyne and Wear Fire and Rescue Service, said: “Saving lives has always been at the core of what we do and crews are used to providing life-saving first aid at incidents. Our trial is looking at how we can extend that work in partnership with NEAS as a part of our clear purpose to create the safest communities.
“Responding to fires and emergencies will always be the top priority for our crews but it makes sense to enable properly trained firefighters to deliver appropriate medical assistance if they can get to the scene first while an ambulance is on its way.”
The trial will run until 30 June 2016 and will be monitored on a daily basis by all parties to ensure it remains an effective scheme offering a level of quality patient care in the local community. Throughout the trial data will be gathered to allow for a full evaluation following its completion.
Caroline added: “At NEAS we are already supported by Community First Responder volunteers who work tremendously hard and do a fantastic job in their local areas. The addition of EMRs will further strengthen our response in these communities and the two models will work side-by-side to save more lives.”
The trial officially launches this month in Tyne and Wear (11th Jan), Northumberland (11th Jan), County Durham and Darlington (11th Jan). Cleveland Fire Brigade, which has been providing this service for a number of years, is extending the service across the Teesside area throughout January.



