Fill our form to download your free research report, written by Dr Mark Hawker.
The Prevention of Pressure Ulcers
The prevention of pressure ulcers and bedsores is a widely discussed topic in the healthcare industry, particularly among those working in hospitals, care homes or looking after people in their own homes.
There are four stages [1] to pressure wounds, however, research has proven that 95% of pressure ulcers in patients are preventable [2] before they reach the first stage, which would save the NHS almost £3.8million in costs per day.
The Stages of Pressure Ulcers
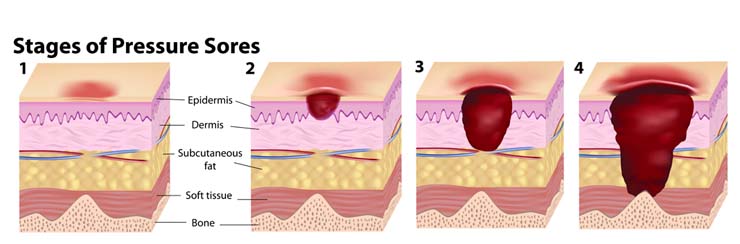
Stage One
Stage one is when the skin is not broken, but there is a sign of hardened, heated and discoloured skin. If pressed the wound remains red and does not lighten or turn white, and after 30 minutes the change in colour does not fade.
Stage Two
A stage two pressure ulcer is when the top layer of skin is broken, creating a shallow open sore. The second layer of skin may also be broken and there may be signs of drainage or fluid leakage.
Stage Three
Stage three pressure wounds extend through the second layer of skin into the subcutaneous tissue below. Although bone, tendon, and muscle are not visible at this stage there may be signs of pus, odor, fever and a greenish coloured drainage.
Stage Four
A stage four ulcer is when the wound has extended as far as the muscle or bone. There will be a lot of dead tissue and drainage present, increasing the risk of infection.
How can they be Prevented?
Pressure ulcers are likely to develop when there is too much pressure on the skin for long periods of time, which often happens with bedridden patients. Not only do they cause pain and discomfort, but stage three and four sores may lead to infections such as meningitis and cellulitis [3], which is why preventing them is so crucial to healthcare professionals and caregivers.
If you or someone in your care is currently on bed rest, there are several things you can do to help prevent pressure ulcers forming.
Changing Position
To reduce the amount of pressure that is applied to your skin over long periods of time it is important that you change your position regularly. It is recommended that people who are confined to bed should change their position at least once every two hours.
If you are unable to change position for yourself a carer or relative will need to assist you, or if you don’t have someone available to turn you regularly there are automatic patient turning systems, such as the Ekamove patient turning system.
Checking your Skin
To help identify the possibility of a pressure wound forming it is crucial to check your skin for warning signs several times a day. It is important to pay attention to problem areas, including your heels, ankles, hips, spine, elbows, shoulders, tailbone, ears and the back of your head.
If you can’t see certain areas of your body easily use a mirror or ask a caregiver to look.
Nutrition

Maintaining a healthy and balanced diet [4] that contains enough protein, vitamins and minerals can help minimise the risk of skin damage to bedridden patients. You may be referred to a dietitian so that an appropriate plan can be drawn up for you, however, the following is recommended to everyone:
- Eat small, regular meals rather than two or three larger meals. If you set a timetable that details when you should eat and don’t wait until you’re hungry, it can help to ensure you receive the necessary nutrition throughout the day.
- Avoid drinking large amounts of fluid just before as meal as it makes you feel fuller than you actually are.
- If swallowing is difficult, try drinking soups, specially made drinks or pureed foods.
- If you’re a vegetarian eat high protein alternatives to meat. This could include cheese, peanut butter, yoghurt, custard and nuts.
Using Pillows or Cushions
Another effective way of preventing pressure ulcers is to put pillows between the parts of your body that will press against each other, such as your shoulders, elbows, knees and ankles.
There are also specialist cushions and pads available that can help relieve pressure for bedridden patients, including mattresses, overlays and heel cushions [5].
Staying Clean and Dry
The cleaner and drier your skin is, the less likely it is you will develop pressure ulcers. Dip a washcloth in a tub of warm water and mild soap to clean your skin with it on a daily basis, lightly patting your skin dry with a towel. Make sure not to rub the skin or massage any treatments into it as it can lead to mild skin irritation.
If you’re worried about either you or someone in your care developing pressure wounds please speak to your healthcare professional. However, if you would like more information on pressure care and preventing pressure ulcers from Mangar, please get in touch to find out how we can help.
References
[1] http://www.msktc.org/sci/factsheets/skincare/Recognizing-and-Treating-Pressure-Sores
[2] http://nhs.stopthepressure.co.uk/Learning/index.htm
[3] http://www.advancedtissue.com/5-tips-for-preventing-bed-sores-in-bedridden-patients/
[4] http://www.nhs.uk/Conditions/Pressure-ulcers/Pages/Prevention.aspx
[5] https://www.drugs.com/cg/how-to-prevent-pressure-ulcers.html
- October 20, 2016
- Bedroom Products
- Occupational Therapists









