Fill our form to download your free research report, written by Dr Mark Hawker.
Frequently Asked Questions About: Falls In The Elderly
Mangar Health is a world leader in the design, manufacture and supply of inflatable moving and handling equipment, designed to safely lift a someone after a fall.
We understand that moving and handling patients can sometimes not only be distressing and undignified for them but can also increase the risk of injuries associated with hazardous manual lifting techniques which is why we advocate the use of safe lifting equipment.
People can have a lot of questions about both falls in general and what to do specifically during and after a fall.
We’ve tried to answer as many of those questions as we could below but feel free to post your own questions in the comments at the end of this article…
What’s The Medical Definition Of A Fall?
A fall is described as ‘inadvertently coming to rest on the ground or other lower level without loss of consciousness and other than as a consequence of sudden onset of paralysis, epileptic seizure, excess alcohol intake or overwhelming external force’ (Source: Close et al 1999, p93).
How Common Are Falls In The Elderly?
It’s obviously possible for anyone to fall over at any time but falls in older people are a lot more common, especially if they have any kind of long-term health condition.
They’re also a very common but often overlooked cause of injury in the elderly.
How Many Elderly People Fall Each Year?
About one in three adults, in the UK, aged over 65, living at home, will have at least one fall a year and half of those will be frequent fallers.
In fact, the most common cause of death in the over 75’s, in the UK, are injuries caused by falls (source: ageuk.org.uk).
What Are The Most Common Causes Of Falls?
Causes of falls come in three main categories:
Intrinsic: These are factors related to the individual at risk of falling such as…
- Previous falls, fractures, stumbles or trips
- Impaired balance/gait or restricted mobility
- A medical history of Parkinson’s, stroke, arthritis or cardiac abnormalities
- A fear of falling
- Medication
- Acute illness
- Dizziness
- Postural hypotension
- Syncope (fainting)
- Reduced muscle strength
- Foot problems
- Cognitive impairment
- Impaired vision
- Low mood
- Pain
Extrinsic: These are factors external to the individual such as the environment they’re in, for instance…
- Stairs and steps
- Clutter and tripping hazards
- Floor coverings (such as rugs)
- Poor lighting, glare, shadows, lack of appropriate adaptations in the home
- Furniture that’s too low to the floor
- No access to a telephone or alarm system
- Poor heating thresholds such as doors
- Uneven access to the property such as high steps, obstacles such as bins, overgrown gardens etc
- Inappropriate walking aids
- Pets
Behavioural Risk Factors: These are factors that an individual may or may not realise they’re doing that contribute to their risk of falling, such as…
- Limited physical activity/exercise
- Poor nutrition/fluid intake
- Carrying, reaching, bending or other risk-taking behaviours
- Inappropriate footwear
- Inappropriate clothing
- Inappropriate use of or refusal to use assistive devices
Why Are Elderly People More Prone To Falling?
There are many different reasons elderly people are more prone to falling but the three main ones are:
- Chronic health conditions. These can include anything, but examples are heart disease, dementia or low blood pressure (hypertension), which all can cause dizziness in a person.
- Impairments: Anything along the lines of poor vision or muscle weakness (which is common amongst the elderly) can make someone more prone to falls.
- Balance Affecting Illness’: Any illness that affects a person’s balance will leave them vulnerable to frequent falls.
How Many People Are Injured Falling Over?
45% of people aged over 65 will be uninjured after a fall but they can cause the person to lose confidence, become withdrawn and feel as if they’ve lost their independence.
The length of time it takes a person to get into a safe and upright (standing or seated) position can have a significant impact on their recovery.
How Can You Prevent Falls In The Elderly?
If you or someone you know are prone to falling, then there are several steps that can be taken to reduce the risk of injury however it should be noted that it’s impossible to prevent falls completely so Post Fall Plans are essential…
- Remove tripping hazards: These can range from the obvious, such as loose lamp/tv cables trailing across the floor, to the maybe not so obvious such as loose carpets, slippery rugs or floorboards sticking up. If you or someone you care for are prone to falls then it’s a good idea to make a review of their home and remove/fix any such tripping hazards.
- Clean up as much clutter as you can: Removing clutter from a home is one of the first things that should be done if someone is at an increased risk of falling. This can include anything from old piles of books or newspapers to oddly sticking out chairs or tables. The less items there are to trip on, the less likely someone is to fall over and injure themselves.
- Try to avoid wearing baggy clothes: Everyone wants to feel comfortable in their own home but baggy clothes, especially anything with a hem that can be trod on, can be a tripping hazard. Any type of clothing that trails on the ground should be avoided.
- Make sure there’s adequate lighting: Poor lighting is another of the major trip hazards that need to be avoided around the home to avoid falling. To design a home that’s more ‘trip-proof’ brighter wattage bulbs should be installed, lamps should be avoided as they can create pools of shadow that might conceal trip hazards and Robert Bunning MD, an associate Medical Director of inpatient services at MedStar National Rehabilitation Hospital in Washington US recommended that night lights be fitted in all bedrooms, bathrooms and halls for better guidance at night.
- Install grabrails: This may sound like an obvious step but having something to hold on to whilst walking around the home or grabbing on to if a fall should occur for stability can prevent a lot of mishaps; especially if the grabrails are placed in positions where falls are likely to occur (such as getting up from a chair etc).
- Wear shoes around the house: Although wearing socks (or going bare foot) around the house is a lot more comfortable than wearing shoes, the grips on the soles of shoes make slipping and falling a lot less likely. If wearing shoes all the time isn’t an attractive proposition, then non-slip socks with grips on the bottom of the feet might be worth investigating; anything that can be done to reduce slipping risks will help.
- Live on one level: Although fitting grab rails around riskier areas can help, stairs will always present a slipping hazard to an elderly or infirm person at risk of falling. That’s why Dr Kaplan, medical director of the Kaplan centre for Intergrative Medicine in Virginia, recommends living on one level. “If it’s not possible to live on one level, try to limit the trips you take up and down the stairs”
- Slow down. Another tip from Dr Bunning it to slow down and take your time as many falls at home are caused by moving from a seated to a standing position too quickly. “All you have to do is pause after going from lying down to sitting and from sitting to standing. Also take a pause before using the railing on stairs, whether going up or down.”
Why Do People Fall Repeatedly In The Same Place?
Falling indoors in the same spot repeatedly is a sign that the above advice isn’t being followed.
It may be that the spot is too slippy or awkward to navigate; it may be that more time needs to be taken when rising from a chair; it may be extra support in the form of grab rails need to be installed.
If a fall does keep happening in the same spot it’s important a Post Falls Assessment takes place and questions such as why did the fall occur and how can falls be prevented in the future are asked and answered to prevent further injury.
Is There A Common Time Of Day When People Fall?
Most falls occur (and extra vigilance is needed) at particular times of the day.
As you might expect, a lot of falls occur either early in the morning when people are drowsy after just waking up and are getting out of bed or late at night when they’re tired and are getting out of their chair to go upstairs to bed.
As we’ve already stated, it’s extra important at these times to go slow, be careful and take frequent pauses to avoid a falls risk.
Other times to look out for are just after medication has been taken.
Many meds can make people drowsy so if medication has been taken it’s a good idea to take it sitting down, in a comfortable spot and just stay there for awhile afterwards until any drowsiness passes.
Are There Medicines That Can Make People Fall More?
Unfortunately, medications are the most common cause of increased fall risk in older people (source: Betterhealthwhileaging.net).
However, they’re also one of the easiest risk factors to change for those that suffer from frequent falls.
If you find you or someone you care for is falling frequently then a medication review with their Doctor or Health Care Practitioner may be needed as part of a falls prevention plan.
Once you’ve identified, if any, medications may be contributing to falls then a falls plan can be put in place to reduce, change or eliminate the use of these medications.
The three main ‘types’ of medication most likely to increase the risk of falls are:
- Medications that affect the brain. Any medication in any way related to the brain, such as for dementia or Alzheimer’s, can have an adverse effect on residents falling. If someone does start to fall a lot, then a review of their medications with their Doctor may well be required.
- Medications that affect blood pressure: Any medication that raises or lowers blood pressure can be a falls risk, especially when rising from a bed, chair or the toilet. This is when a person is most likely to feel dizzy and is called postural (or orthostatic) hypotension which can lead to a fall; so, if this is happening a lot a medication review may be performed as part of a post falls assessment with the pro’s and cons of taking/changing the medication being weighed against the number of falls occurring.
- Medications that lower blood sugar levels: The final type of medication that needs to be considered in a fall’s prevention plan is anything that can lower blood sugar levels. This only really applies to people with diabetes but as that’s 3.7 million people in the UK (source: diabetes.org.uk) it’s a pretty big number to consider. Hypoglycemia or low blood pressure, is when the blood sugar levels dip below their normal range. This can then result in a variety of symptoms which include clumsiness, confusion, loss of consciousness and seizures all of which may result in a fall. As with blood pressure medications a falls assessment would need to be conducted with a Doctor to weigh the pros and cons of the medication when weighed against the frequency and severity of the falls
What Can Be Done To Prevent Falls When Outside?
We’ve already discussed what can be done to prevent falls in the home environment but people wont always be in a safe, controlled environment like their home when they fall.
So what can be done to prevent or limit falls when a person is outdoors?
- Select the right shoes: It probably goes without saying but high heels are to be avoided at all costs but it’s also worth getting rid of any shoes with too thick a sole as they don’t provide the stability needed to keep an even footing if someone’s unsteady on their feet. Instead look at footwear with a thinner, non-skid sole (source: National Osteoporosis Foundation). Lace up shoes are also much safer than slip-ons as they allow for a tighter, more fitted ‘fit’.
- Slow down: This is the same advice given for when moving around indoors but is even more important when out walking on a variety of different surfaces or in different weather conditions. A great piece of advice it to try and add time to the journey if there’s a rush. If a journey would normally take five minutes allow for ten so more time can be taken to be more careful.
- Always pay attention: Again, a lot of this advice might sound obvious but how many of us listen to music whilst walking the dog? Or talk on the phone as we’re walking to the shops. Whilst this isn’t an issue for the majority of people, those that are at an increased risk of falling need to be more aware of their surroundings, where they’re walking, where they’re putting their feet etc.
- Assess all surfaces: Much as we said in our previous piece of advice, pay extra attention when moving from one type of surface to another if there’s a risk of falling. Walking into a shopping centre with slippery marble floors for instance or a restaurant with polished hard wood floors or practically any surface after it’s rained. When moving from one surface to another a moment needs to be taken to evaluate it. Placing one foot on the new surface and rubbing it back and forth can help with getting a firmer footing. It may feel a little silly but it’s a lot better than taking a tumble!
- Be careful of curbs and steps: Steps and curbs are some of the worst trip hazards when walking outside, especially when you consider falling out into a road! They all tend to be of different heights and even when the curb has been lowered there will be a slope that needs to be taken into account. Take your time and take it slowly.
As a final piece of advice, if returning home after dark is a frequent occurrence then leaving a hall light on helps to see better on the approach to the front door as there can often be pools of shadow that are easy to trip in. Or better yet have an outdoor motion sensor light fitted that will come on automatically.
What Equipment Can I Buy To Help Prevent Falls?
When it comes to falls equipment there’s two main categories to consider; equipment to help people back up after a fall in a safe and dignified manner and equipment to help prevent falls in the first place. For this question we’ll be focusing on the latter…
- Slipper Socks: We know we’ve already talked about slipper socks with grips on the sole but we really can’t stress how important they can be around the home. Having a firmer grip on the floor, especially on different surfaces (carpet, wood, lino, tiles etc) really does make a difference to the frequency of falls occurring.
- Grab Bars: Again, we know we’ve already mentioned grab bars but placing them strategically around the house in places where extra help is needed is vital in preventing falls.
- Toilet frames: A lot (and we mean a lot) of falls occur when getting up from the toilet. These falls can be particularly awkward as most toilets are such a confined space that it can be very awkward to help someone up. Toilet rails (like grab rails but on either side of the toilet) can help prevent this by providing a lot of extra support when getting up from the toilet.
- The Mangar Raiser: Over 12,000 people each year are admitted to A&E after falling when trying to get out of their chair and more falls happen in the living room than anywhere else in the home. The Mangar Raiser is a portable, inflatable cushion that can be placed on a seat that then helps take people from a sitting to a standing position. It’s also portable enough that it can be used in a car, in a wheelchair or be taken on holiday. You can find out more here >>
- Crash Mats: Crash mats don’t really come under the term falls prevention and don’t help people up after a fall either. What they are great at however is preventing injury. A falls crash mat is exactly what it sounds like. They’re thick, padded cushions that can be placed on the floor next to a bed or sofa so that if someone does fall the padding can soak up a lot of the impact force, lessening the risk of an injury after a fall.
What Should I Do If I Find Myself Falling?
So far, all our advice has been about the prevention of falls but no matter how hard you try you can’t ever completely eliminate the risk of falling.
If a fall does occur it’s important to try and fall ‘correctly’ to minimise/prevent any injuries that you might sustain.
- Try to protect the head and face: Damage to the head and brain can be one of the most dangerous outcomes from a severe fall so to protect the head from impact damage try to keep the chin up and protect it with your arms as the fall occurs. An often-overlooked source of injury from a fall is biting of the tongue. In a fall try to keep the tongue firmly on the bottom of the mouth, behind your lower row of teeth to avoid biting it when you hit the floor.
- Roll to safety: The risk of injury whilst falling can be mitigated somewhat by tucking up into a ball and rolling. This avoids damage to fragile body parts like the head, wrists or hips and rolling as the ground is hit spreads out and absorbs some of the force from the fall.
- Avoid dangerous objects: It’s easier said than done but if dangerous objects such as sharp obstacles or broken glass (more likely if the fall occurs outdoors) are underneath/around then an attempt should be made to try and push away from them as the fall happens or by quickly rolling when landing. If it’s not possible to do this then covering the head and face with the arms helps to protect this sensitive area.
- Relax the body: Humans are only born with two innate fears; the rear of loud noises and the fear of falling; all our other fears are learnt behaviour. This means that when we do fall we tend to tense up in a panic which is actually one of the worst things that can be done. Tensing up causes more of an impact by increasing resistance and torsion which adds more injury to the falling body. Trying to relax and letting the limbs stay loose when falling, especially the legs, helps reduce this damage.
- Hit the ground with a flat palm and the forearm: When falling it’s important to protect joints such as the wrists as much as possible. The temptation will be to try and land with the hands down to break the fall. When falling in this way splaying the hands out flat and landing on the palms and forearms helps to absorb more of the shock and help prevent injury (source: com).
What To Do After A Fall If You Can Get Up…
After a fall one of two things are likely to happen. Either the person who has fallen will be able to get up on their own or they won’t be able to. If there’s no injuries after the fall then the safest way to get back up is to…
- Lie on your side, bend the leg that’s on top and lift yourself onto your elbows or hands.
- Pull yourself towards an armchair or other sturdy object around you then kneel whilst placing your hands palm down on the chair or object.
- Place your stronger leg in front of yourself, holding on to the chair or object firmly.
- Stand up by applying pressure downwards with your palms and stronger leg.
- Very carefully and very slowly turn and lower yourself into a sitting position.
- Most importantly, stay calm throughout the entire process.
What To Do After A Fall If You Can’t Get Up…
If the person who has fallen is in any discomfort or pain and/or are unable to get up, then help needs to be sought…
- Call out to someone if you think you may be heard
- If you’ve an emergency call device or mobile phone on you then use it.
- If you don’t have either of these try to slide yourself towards a phone or a place where you’ll be more easily heard.
- Make as much noise as possible around you with a walker or any other object to attract attention.
- Wait for help in the most comfortable position you can get yourself in.
- If you’re able place a pillow under your head and cover up with a piece of clothing or a blanket to stay as warm as possible.
- Try to move your limbs/joints as often as you can to ease circulation and prevent painful stiffness from developing. (source: phac-aspc.gc.ca)
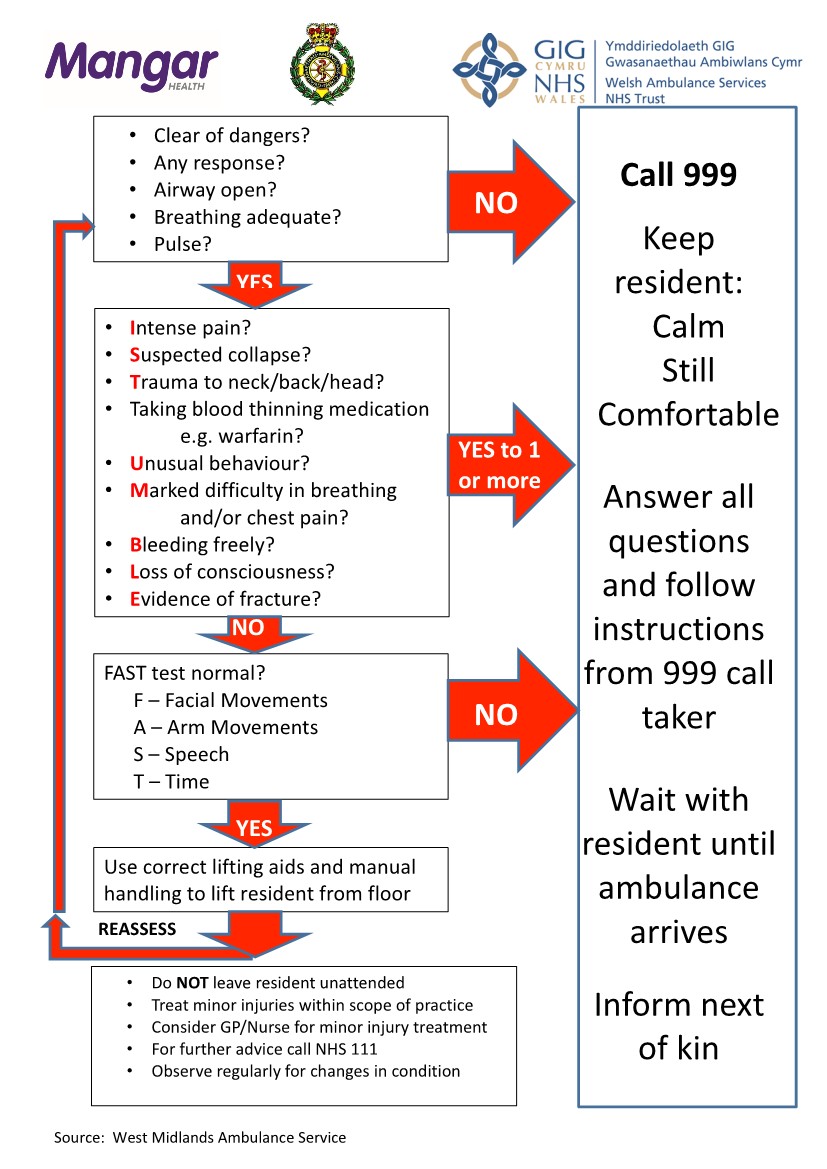
What Should I Do If I See Someone Fall Over?
If you see someone fall over it’s important to resist the urge to help them straight back up as this can cause a lot more harm than good, especially if they’ve broken a bone.
Fortunately, West Midlands Ambulance Service has released a guide called IStumble for exactly this situation with a simple flow chart showing if it’s safe to lift someone after a fall or not.
Should I Call An Ambulance After A Fall?
The NHS website provides great advice on when it’s appropriate or not to call 999 after a fall…
- Has there been loss of consciousness?
- Is the person in an acute confused state?
- Are they having fits that aren’t stopping?
- Is there chest pain?
- Are they having difficulty breathing?
- Is there severe bleeding that can’t be stopped?
If the answer to any of the above is yes, then 999 should be dialled straight away.
But… if either yourself, or someone you know has fallen and are uninjured (as is the case in 45% of falls in the over 65’s) then other options should be considered before calling 999.
If there’s no injuries after the fall then our previous advice can be used to get up either alone or with the help of someone else.
If there’s no injuries but the person is unable to rise themselves or be helped up then a call to NHS 111 is needed to arrange for a Falls Team or Community First Responders crew to come out and lift them rather than an ambulance which may be needed for more serious incidents? (Source: nhs.uk)
What Equipment Would The Ambulance Service Use To Pick Someone Up Off The Floor?
If you’ve fallen and are unable to get up and an ambulance is on its way, then it’s reassuring for a lot of people to know exactly what will happen next.
All Ambulance Trusts in the UK use a device called the Mangar ELK which is an inflatable Emergency Lifting Cushion to get someone who has fallen over back onto their feet.
You can see the Mangar ELK in operation below…
If they know they’re a frequent faller many people even have these at home themselves to get back up after a fall rather than waiting for an ambulance and if you’d like to learn more about having your own Mangar ELK at home you can do so here >>
What Are The Most Serious Consequences Of A Fall?
There tends to be two different consequences that occur after someone falls. Those are the physical and then the mental effects.
Physical symptoms are easiest to describe and can include:
- Broken or fractured hips, femur’s, pelvis or vertebrae
- Broken or fractured humerus, forearms, hands and wrists
- Broken or fractured leg and ankle bones.
Some fractures that occur after a fall can obviously be more serious than others with hip fractures causing the greatest number of problems.
That’s why we’ve spent so long discussing preventative measures to avoid falling when at home or outdoors.
Whilst getting older does increase the likelihood of a fall, the longer you can prevent them or minimise their impact to your life the happier and healthier you’ll stay.
How Long After A Fall Is It Safe To Be On The Floor?
It’s essential to get someone up from the floor after a fall as soon as possible as long lie (as it’s known) can lead to serious health complications which will negatively impact a person’s quality of life.
Within most official Post Falls plans there are two timescales defined for someone being left on the floor:
- Delayed Initial Recovery: This is defined as a lie (being left on the floor) greater than ten minutes but less than an hour
- Long Lie: This is a lie that’s greater than one hour after a fall.
Consequences of a long lie post fall can be severe and range from:
- Muscle damage
- Hypothermia
- Dehydration
- Incontinence
- Pressure sores
It also gets worse. 20% of patients that are admitted to hospital after a fall will have been on the floor for at least an hour and of those 50% will be dead within six months, even if they were uninjured in the original fall (Source: Vellas et al).
And once someone has had a fall there’s a 60% chance they’ll have another!
This is why it’s vital to make sure the time someone spends on the floor post fall is minimised as much as possible.
I’m Very Anxious About Falling, What Can I Do?
Perhaps worse than the physical effects a fall can have on a person are the phycological effects, as they can often cause a vicious circle in an individual.
When a person falls for the first time it’s quite natural (and even understandable) to develop a fear or anxiety of falling.
This can then result in them leading a much more sedentary life, staying in a chair for much longer periods for instance, to minimise the risk of falling.
The problem is this reduced mobility/sedentary lifestyle means there can be additional weight gain through lack of exercise, an increase in blood pressure and a loss of muscle mass all of which are contributing factors to falls in the elderly. Another fall then occurs and the cycle spirals downwards.
If you do feel this applies to you or someone you know its important to try and increase confidence levels.
- As per the advice in this article, identify when a person is falling and take action to reduce the risk.
- Make a plan for getting help if they should fall.
- Make sure they talk to someone about their fears and anxieties.
- Set small achievable goals to help them feel more confident again.
- Challenge any negative thoughts.
- Keep as active as possible.
- Practice relaxation techniques.
Facts About Falling
- Around one in three people over 65 and one in two people over 80 fall at least once each year
- Falls account for around 40% of all ambulance call-outs to the homes of people aged over 65 and are a leading cause of older peoples use of hospital beds
- Each year there are around twice as many fractures resulting from falls as there are strokes in the over 65’s
- Falls are a common reason for people moving into long-term care or needing more help at home
- Each year 75%-80% of falls go unreported
- For people over the age of 75, falls are the leading cause of a permanent disability
- A person is three times more likely to fall in a care home or hospital environment
- 86,000 hip fractures per year (95% of all hip fractures in fact) result from a fall
- 640,000 presentations to A&E departments each year are as a result of a fall
- Falls that result in a hip fracture cost the NHS around £2 Billion a year
- Everyday 500 older people are admitted to hospital because of a fall; 33 of them will never go home
Do you have any questions about falling we’ve not answered here?
Feel free to post them in the comments below for us to answer…
- November 08, 2018
- Care Home
- Dementia
- Occupational Therapists
- Patient Lifting Products










A very helpful article
What are the risks/consequences of moving someone who has been on the floor for days, in relation to then allowing them to sit up or stand and the risk of toxcisity from rabdo? Especially in relation to cardiac or kidney damage. Thank you
Rhabdomyolysis is not that common in patients suffering a long lie alone, unless there is associated traumatic injury. In cases without traumatic injury it is common that symptoms do not develop immediately but after several days so you would not know if the patient is suffering Rhabdo at the time . Any traumatic injury should be picked up thorough initial primary assessment (iStumble), and 999 would have been called minimising the risk of a long lie.
Generally if there are any mild signs of Rhabdo through a long lie, such as muscle cramps, weakness or tiredness within 48-72 hours medical advice should be sought and diagnosis will be made by a healthcare professional.
In respect of moving a patient after a long lie, if there are no signs or symptoms of Rhabdo then the patient is safe for lifting using correct techniques and equipment, but if there are any red flags, 999 should be called as ECG’s and blood tests are required to be able to reach a correct diagnosis.